Category: Chemotherapy for Myeloma

June 26th, 2020 by Janine
You are a bit of bitch really aren’t you? Very clever. Coronavirus, Covid19 or whatever you are calling yourself, you’ve sent the world in to a tail spin. You’ve made it even harder for those with less and caused loss, grief, fear and stress to many. You’ve caused economic chaos just when the country’s debt was coming under control. Corona1, you have brought the best and the worst out in people. You’ve given the scientists, statos and health analysts a right royal challenge to get their teeth into. I hate you. I don’t want to die from Covid19, Cancer already has that sewn up. I’m cool with that. You on the other hand are ruining my precious life. Now bugger off.

Coronavirus Care Bear
Hospital
Every week when I’ve gone to hospital for chemo, had my blood taken and received an injection, I’ve risked catching you! My body perceives such a high threat level that is on edge the whole time I am there. I am antsy when I have no choice but to walk down corridors where physical distancing is impossible. I wear double masks, I wash my hands constantly and in my mind you hover on every surface, everyone’s lips, everyone’s clothes. I cringe with every sneeze and cough heard. My body is so hypervigilant and tense that when I finally get out of the hospital I am thoroughly exhausted.
You, Corona, are a cruel cruel virus. I took time to focus on being as well as I could during my current cancer treatment and to foster as much calm as possible. Huh! Calm is very hard to come by most days thanks to you, let alone on hospital days when it is nigh on impossible to feel relaxed.
Strangers
I was trying to get my head around you Corona and your ramifications, for my bubble of hubby and me, for my loved ones, when strangers suddenly became very scary entities. Minding my own business in a hospital corridor, a man walked towards me, looked me directly in the eye, shook his head seemingly disapprovingly and then, coughed. He coughed again, purposefully. He looked directly at my face, coughed a third time and then with his hands hurled his cough at me. I was shocked and almost stopped. He threw his head back, laughed, looked at me again and grinned. Then he carried on as if nothing had happened. So too did the person behind him.
It was over in seconds. My thoughts raced – is that it? Corona, does he know you have infected him? Did he want me to get sick? Why? What did I do? Isn’t having cancer enough? This happened the week before official lockdown here in the UK. If it was your idea of a practical joke Corona, you got me. I was worried for weeks, waiting to see if you had landed, were going to take my breath away, make me very very sick or you know, kill me.
Assault
Once in lockdown, this incident would be called assault. The man could be found, arrested and charged. I would report it. At the time I didn’t know this and it was the last thing on my mind. I was in shock, kept walking and found myself trying to work out what had just happened and why. I remember feeling and thinking that somehow he had taken offence to my looks or seeming wealth. I had my headphones on and was listening to a podcast, he looked dishevelled and possibly impoverished. Did he think me too wealthy, too fortunate? Well I am fortunate in so many ways however that doesn’t excuse his or anyone’s attempt to cause me harm.
On reflection Corona, I realised there could be a million reasons why he did what he did, none of which might match with my first interpretation. I would never know his rationale so there was no point me thinking about it anymore. Yet somehow, Corona you had made me a target, when I already was one, thanks to cancer. You forced me to think about a whole heap of virus stuff that I really didn’t have a lot of headspace for. Instead of hospital being safe, the place I go to heal, you have made it a very scary destination.

Thanks a bunch Corona.
No more adventuring
Maxed out vulnerability. People living with (or dying with, if its a bad day) Myeloma are in the seriously at risk group. If I followed the full UK guidelines to the letter, for people who need to shield, I wouldn’t be sleeping in the same room as my husband, spending time in the same room as him, cooking and eating with him. I would be alone in a bedroom, only allowed out for bathroom breaks and to use the kitchen separately. That wasn’t go to work. Not unless one of us got the virus or hubby had to go out of the house a lot. You almost stuffed up my home life Corona. You certainly stuffed up my adventuring (two cancelled trips that I was so looking forward to and that would have balanced out being on crappy treatment) . No, you were not going to get it all your own way.
Best bits
Lockdown hasn’t been all bad. Consistency has been my main word, mantra, possibility, call it what you will. I committed to myself to choose somethings I would do while unable to go out and do them consistently. In fact, you gave me a renewed sense of purpose, a new start line. I checked in with myself, wrote a list of things I wanted to do and began chipping away, doing a little bit of one thing each day until it was complete before moving on to the next task. Thanks to being stuck at home with less outdoor distractions I’m feeling good about lots of little and not so little achievements. Cheers Corona.

Not us (obvs) but cool pic
My new morning routine makes me feel great. I re-established my intake of a litre of water with lemon juice, my herb drink and added in yoga. Hubby and I completed two 30 day yoga programmes and are part way through another with my favourite online teacher Adriene from Austin, Texas. (links at end). My downward dog is the bees knees. My hip flexors on the other hand….are getting there. I’m loving it.
For the first two months I cycled on an indoor bike at least once a week, paced the length of the garden until I got dizzy or had listened to hours of a podcast and worked out with weights. I felt stronger and healthier than I had in an age. I finally submitted two research papers to journals for peer review (core topics: dementia, family involvement, interventions). Another paper I was involved with, was published. Manual client notes from work completed prior to using a record system are now online. My continuing professional development log is up to date. It even contains new entries from the multiple courses I’ve down during lockdown. I’ve enjoyed growing my Acceptance and Commitment Therapy (ACT) skills.
I baked gluten free, natural sugar only, snacks and slices that all turned out to be edible (by me at least). I cooked loads and cleaned like I had never cleaned before. Well that’s not true (some of the end of tenancy flat cleaning days were mammoth) but I cleaned more thoroughly than I had in an age.

Silver Rooster Easter Bonnet

Blurry Bonnets!
I’ve kept in touch with loads of friends. Had virtual drinks and dinners, coffee catch ups and laughs (especially over the Easter bonnet competition which included a plane and a silver rooster, no less). Had friends drop off yummy treats and delicious fresh fish. Clapped for the NHS and frontline workers. Formed deeper connections with my neighbours through whatsapp about shopping, helping out, puppies, compost, birthdays and more. Learned about tiktok, seen some things about Trump and some other dodgy characters that I never want to see again! Corona you have forced a new world upon me and I will remember the bright spots. Even though….

low day(s) duvet day(s)
Limits
You almost got me. My mental health took a hit. I made it to about day 50 when cabin fever hit. Half way through the worst 24 hrs Corona, I discovered my knickers were on inside out. I didn’t care but it did sum up the day.
You are scary but I was over being home. I was desperate to go for a long walk. My right hip was giving me grief and I knew walking would help. In early March, my hip decided to drop and rotate forward (it’s done this before). Joy of joys. You didn’t care Corona. You had your own schedule. Before I could book a physio appointment to feel the relief of alignment you made everyone stop work and close doors. No face to face let alone hands on work was allowed. My body hated you.
My hip got steadily worse. The pain was constant, worse when I sat down or lay on that side. I felt like one of those bobbing dog toys hanging from a car driver’s mirror; up, down, side to side, up down, side to side. I’m surprised hubby didn’t slip me something in a cup of coffee so I just stayed still for a few hours.2

Joyden Woods Walk
Latest
Dr B gave me permission to leave the house!! As long as I avoided everyone. He wanted my mental health to be ship shape because the next step of treatment is a tough one. I woke up early. There was no one about. I put my masks on and walked. Walked for an hour. I breathed deeply. It felt so so good. Ha Corona. Take that!

Despite you, the pain in my hip is now improved and I’ve completed another seven months of chemo.3 OK my consistency has gone to pot over the last two weeks but part of me loves that; I’m human after all and needed to rest my painful hands and wrists. Even so Corona, your attempt to disrupt my treatment, health, heart and hope has been futile; I’m ready for the stem cell transplant (SCT).
It does look like I’m going to have to do the SCT alone. Without face to face visits from hubby or friends to make me laugh and just be with me. Corona, you had to have the last word didn’t you? You really are a bitch.
——————————————-
1 I can’t get the chorus from My Sharona (The Knack) out of head so Corona, my nick name for Coronavirus/Covid19 stuck, sorry.
2 Not a joking matter I know.
3 A quick update on this to come in another blog
Great yoga sessions and teacher:
https://yogawithadriene.com/
https://www.youtube.com/c/yogawithadriene/videos
Acknowledgements
Unsplash Images:
Sarah Kilian – Bear with Mask
Robin Benzrihem – maskonground
Robert Collins – man_woman_dance shape
Mika Baumeister – thinkingmask
Jurien Huggins – duvet
Ashkan Forouzani -stayhome
Anastasiia Chepinska – ClosedCovid
Other images:
Others – Me & Hubby

© 2020 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Chemotherapy for Myeloma, Covid Tagged with: Cancer, Coronavirus, Covid, Covid19, Lockdown, Mental Health, Virus, Yoga

February 12th, 2020 by Janine
I listened to an interview with best-selling author Marion Keyes today and she talked about writing emotional landscapes. This is a wonderful phrase; it captures the many random thoughts I have about life, being human, living with cancer, with chemo, with uncertainty. Random thoughts, the theme for this blog, a collection of moments from the last two months where thoughts appeared in my mind as I sat, walked, waited, tossed, turned, fumed, cried, ached, appreciated, smiled, laughed and loved, always loved.
Music

House music is on my mind and in my ears…though the Brighton weekend for clubbing was a bust – great weekend – we just didn’t find a stylish club with fab house music. Our guys went ahead to do reconnaissance. They didn’t even make it inside one club. A group of people came out (not fast enough according to them) saying very loudly how sh*t the club was, dark, dingy, crap music…needless to say we abandoned that idea. Fab friends made up for clubbing disappointments. After all, we are fortunate enough to live in one of the best club cities in the world so maybe we’ll stay local next time!
Chemo Update

The chemo regime called VTD is different this time, cannulation monthly only – yippee! The weekly injection of Velcade isn’t so bad. I take one dose of anti-nausea beforehand and haven’t needed anymore anti-nausea drugs afterwards so far. I end up with a little localised bruising. The drug kicks in fully after about 36 hours…funny sensations, aches, pains (all bearable) in my bones…I visualise Myeloma shrivelling and dissolving.
The Thalidomide seems to impact my quality of life a lot more than the Velcade. Yes that Thalidomide, the one that causes horrible side effects for foetuses. It is no longer given to pregnant women but was discovered to have a positive impact on cancer, see here), The daily 80mg dose knocks me out and I feel tired ALL THE TIME. The stuff is toxic. A nurse who first administered the pills to me was gloved up and handling it like it was a hot potato, doing their best to avoid all contact with the pills. I wondered what the hell I was about to put into my body!
Even the weekly steroid doesn’t combat the lethargy (but it has made me eat more and I’ve put on 7kg that I don’t want!). Early morning energy is now a distant memory. The other unwanted side effect of is my stomach is like a horizontal crackerjack. I take Thalidomide and out my stomach comes, tight and large, making me look like I have consumed a whole loaf of gluten filled bread or more ironically, I look pregnant. On top of the VTD chemo regime I inject nightly Clexane, a blood thinner to stop the Thalidomide from causing blood clots.
Oh the layers…take this because it helps this but then take that because to take the first thing you need that thing to stop the bad things of the first thing….and round and round it goes….Still, the regime is working and the presence of Myeloma in my blood and bone is dropping again, down from 17 to 11. Hopefully it will continue to fall.
Creepy Chrimbo

Doesn’t it seem an age since Christmas already? I nicked named last Christmas, Creepy Chrimbo because the hospital was strange and very different from usual. My chemo didn’t stop just because it was Christmas eve or New Year’s eve. I am grateful for all of the hardworking nurses who managed to fit in everyone’s treatment to a short week so Christmas Day could be the best it could be.
Hospital halls were eerily empty and I could hear every footstep I made ringing in my ears. I felt like I was in an Alfred Hitchcock thriller or that Jack Nicholson’s horror film grin would appear around a door jamb any second. The sense of being alone was made worse because the Chemo Unit is down the end of a long corridor, I often feel like it’s ‘shoved away’ with the renal unit, out of the way because somehow we are toxic and ‘they’ don’t want us near others, the healthier people, in case we contaminate them somehow. I know this is silly but then maybe not? Chemo is after all, hazardous, noxious and needs careful handling so maybe it is purposeful that our unit is past the research centre and beyond the other wards. I know it isn’t helpful to think this way, a little negatively, like we are not really wanted and are merely being put up with somehow. The NHS staff certainly don’t perpetuate this story; they are friendly and welcoming.
Just before I was alone in the long corridor I noticed a woman on a hospital bed being wheeled towards the renal unit. I try not to look at people when they are being wheeled around in public view, I often think it is fairly undignified yet obviously a necessary event in hospitals. I wouldn’t want to make eye contact with anyone if it was me on that bed. I’ve noticed some patients close their eyes, put a pillow or blanket over their face – possibly to gain some privacy in a very public space so I try to offer it by glancing away quickly. Though if someone in a bed looked directly at me I have decided to smile and hope they find it reaffirming, reassuring, and non-judgemental somehow.
This woman was on her side, looking away. It was after 5pm on the 24th and I wondered what her Christmas would be like and what her story was. Would she be sad to be in hospital over Christmas Day? Did she have family who wished she was with them? Would they visit her? Did she want them to visit? Or was she secretly relieved she had the best excuse to not ‘do’ Christmas this year, to rest and focus on herself instead. Or maybe she didn’t celebrate Christmas at all and instead would be disappointed to be missing out on holidays. These thoughts vanished as I found myself alone in a grey corridor with white walls, in silence where there was usually the hustle and bustle of nurses, doctors, patients and public, trolleys and endless supply boxes.
The silence strangely continued outside where the usually busy main street was devoid of cars and people. This reminded me of the contrasts of Christmas, wonderful, fun, exciting for some and challenging, triggering, or lonely for others.
Repurposed

The new buzzword popping up everywhere is Repurposed. From transforming old furniture into something new or turning one person’s rubbish into another person’s useful item, and now, the latest thing is repurposed drugs. Essentially, using drugs already approved by the medication regulators for treating non-cancer illnesses, to treat cancer or be added to existing cancer treatments to increase effectiveness.
When I first came across this I thought it was yet another cancer fad because the headlines gaining traction were about repurposing dog wormer! Yes you read correctly. Cancer patients were shouting out about how an anti-parasitic drug called Fenbendazole usually used for deworming dogs had cured their cancer! I was very dismissive. I don’t want to miss out on something that works but I don’t want to get caught up, distracted, invest time and precious energy into the cancer equivalent of the latest diet or beauty treatment. Dog dewormer seemed to be more in the fad than the credible category and on par with ‘take turmeric’ and your cancer will vanish. While I am a big fan of turmeric and curcumin and take it daily, I do not believe for one second that it (or Fenbendazole for that matter) will single-handedly cure my cancer or cure anyone’s cancer.
But then I got thinking, had I been too quick to write off this idea? Medical discoveries come in many forms, (like the Thalidomide scandal) from unlikely places so why wouldn’t it make sense that a medication that addressed one illness, whether in animals or humans, might also be found to have anticancer effects? I took another look and found this. Click Here
I googled some more (as you do) and came across some other interesting stuff…
Trials and projects involving existing non-cancer drugs are now being investigated for their effects on cancer – these are so important because if found to be effective they are likely to be approved for cancer treatment quickly, be cheaper and more widely accessible as they are already approved for human use and side effects are known. These links explain more..
https://integrativeoncology-essentials.com/2020/01/use-of-off-label-drugs-and-supplements-in-cancer-in-2020/
http://www.redo-project.org/
Imagine living with cancer, walking in to a clinic, having your DNA and genome sequenced by a friendly lab technician and walking out knowing a specialist will create a cancer killing virus tailored just for you and your cancer. This is another exciting development that doesn’t seem too far away now…it’s not science fiction! Check out Andrew Hessel, founder of Humane Genomics, he explains how tailor-made viruses may one day cure cancer.
https://www.youtube.com/watch?v=2jjQ4QDhuBU
I wonder how I will be repurposed…will I be fertiliser for a beautiful oak? Will I return as a stretchy, wiley happy cat? A roll of loo paper (someone’s revenge though at least it’s useful)? Or a spider, imagine eight eyes to people watch with….
Contract
I’m due an upgrade on my phone. Chatting with my wonderful friend and hairdresser K, we laughed about our mobile phone providers and how I could easily be expected to sign up to a new contract that would out last me! Humour and especially dark humour is an emotional landscape I find really helpful.
Blue Sky
It is a high blue sky, crisp cold and sunny day in London today. This emotional landscape is beautiful and I found myself smiling, A LOT.

Acknowledgements
Images:
Woman in the woods – Andrew Neel on Unsplash
DJ – Jernej Graj on Unsplash
Dog Wormer picture (care of The Sun)
Others – Me & Hubby
© 2020 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Chemotherapy for Myeloma, Myeloma Treatment, Results Tagged with: Bone Cancer, Cancer, Christmas, Dexamethazone, Dog Wormer, Drugs, Fenbendazole, House Music, Myeloma, Repurposed, Steroid, Thalidomide, Velcade

Peripheral neuropathy. A fancy pants way of saying pins and needles. Except it is a bit more than that and the more, is scary. When tingling on the soles of my feet and in my hands turned to prickles and cried out for attention, I had just started my 14th cycle of chemo. At night, as if hedgehogs at a rave, the prickles began dancing around, keeping me awake. My self congratulation for having coped well so far and immense gratitude to my body now seemed a little premature or at least to have jinxed me. A strange oscillation between numbness and pain set in. At first, it came and went so I wasn’t too worried. I kept up the once a week, Maintenance Chemo.
Pain
The pain got worse. The tingling turned to a sharp micro needle feeling and the ache crawled up my left arm. I remember thinking, this isn’t good. I started talking to hubby about wondering whether the benefits of chemo still outweighed the side effects. We decided they did. I kept going.
So, did the sensation and the pain. The cannula insertion became excruciating. The drip of the drug into my forearm was ok but by the end of the treatment the whole arm throbbed; I hadn’t had that before. In the days in between chemo, the pain, numbness and needling rollercoaster, deepened and didn’t let up. I felt increasingly fatigued, distracted and unable to concentrate. Pain will do that. The symptoms eased a little if I did nothing and stopped using my hands altogether. Have you tried that? It is nigh on impossible! My weekends became slow, sedentary, dull; low mood came a calling.
Peripheral neuropathy doesn’t like hands
Then it hit me; the way I hold a pen had changed. The length of time I could hold a hairdryer and the way I used a hair brush had changed. Whenever a cap needed to come off a bottle, I now ask for help. I was using two hands to open doors or press flush buttons on toilets. Cooking had virtually stopped (and I had thought I was being lazy) instead lifting chopping boards, holding pans, taking roasting dishes out of the oven were difficult. I no longer enjoyed being in the kitchen. No wonder I’d started avoiding it. Hubby rattled off a list of other things I’d stopped doing or was doing differently.
I felt exhausted just thinking about it. Should I stop treatment? Should I keep going? Would I lose the use of my hands if I continued with chemo? What would life be like if I couldn’t use my hands? If the pain was too much? Was I being a wimp? I’m on a clinical trial, I signed the forms, I committed to it; could I simply stop? What would happen to me if I did stop? Would my cancer flare? Was chemo worth it? Was chemo making things worse? How do I decide whether to continue something that may extend my life, when it seems to be significantly reducing, the quality of the life, I have left? My brain; the whizzing and often unhelpful thought production machine, joined the rave.
Holding pattern
I told my oncologists what we had noticed about the difficulty using my hands and how I was questioning whether to stay on the trial; questioning whether more chemo was the best thing for me. They ran a few tests and determined I had lost strength in my hands, especially my left hand. They recommended I defer chemo for a week.
That week came and went with no improvement. I went into a holding pattern for another week. Peripheral neuropathy is the pits and as well as dancing needles it feels like being burnt, a searing. The pain was constant, in my shoulder, my forearm and using my hands made everything worse. More MRIs were ordered. I started to worry about new lesions. Was it peripheral neuropathy? Would it get worse? Was it something else?
Deal or no deal
It came down to one week and the limit of missed weeks allowed when on the trial. I had happily missed a few weeks of treatment to be with Mum during part of her radiotherapy and then missed additional weeks while we waited to see if the pain and hand function would improve. We now had to decide, the medical team, hubby and I, the best next step for the one remaining week; chemo or no chemo. Sounds like deal or no deal except there was no money involved, no windfall or good luck, instead hope or no hope. Bones versus hands.

Hands won. Living rather than life, won. This time. Drs L and A recommended I stop chemo; they didn’t want my hands to get worse and so I was kicked off the trial.
After 21 months, 17 cycles of chemo, virtually weekly blood withdrawal, 100 odd cannula insertions…it was time to give the body a break.
Care as Usual
I went off the trial and on to ‘care as usual’. What I didn’t factor in, was that meant I would no longer be looked after by the trial team, the team that had had my back from the beginning, the team I had come to know, feel safe with, could express my fears and questions to and laugh with. I would be losing the team that had been with me since March 2017 when I first stepped into the Chemo Day Unit and steeled myself for the uncertainty of cancer treatment. Sigh.
Then of course there were the dominos. The other life challenges, falling thick and fast. Not sure what I mean? See my last post, Silent Dominos.
So while still dealing with Mum’s recovery and ‘what next’ (she’s amazing by the way) and my peripheral neuropathy and hand malfunction… along came the next three dominos:
- Changing treatment, care team and feeling cast out into a new uncertain hospital process
- Dad’s Melanoma came back
- My cancer got worse
Who on earth had it in for my family? Who had we unintentionally, unwittingly, annoyed?
All of us with cancer. At the same time.
We didn’t deserve this. No one does. I needed to remind myself:
Cancer doesn’t care who you are or what you have or haven’t done. It’s simply not that choosy.

Posted in Cancer in my family, Chemotherapy for Myeloma, Myeloma Treatment, Pain, peripheral neuropathy, Symptoms and Side Effects Tagged with: Cancer, Chemotherapy, feet, hands, Myeloma, peripheral neuropathy, pins and needles, Side effects, Treatment

April 18th, 2018 by Janine
Sick as a dog, thank you Chemo. I am meant to be on top form tomorrow. It’s hubby’s very special birthday and we have a full day of fun planned. Thanks, thanks a million for deciding to be ‘a bad Chemo’ day. Team, my wonderful team, I feel let down. There has been a mistake. You forgot to give me my steroids. I trusted you. I felt safe. I wasn’t safe today. It made a difference, a huge difference. I let myself down too. I forgot to do my own checks. I forgot to ask for my steroids. Consequences. There are always consequences in this Cancer game, some big, some small, some easily remedied, others drastic and most, a right pain in the arse. Consequences, you can rip the rug right out from under my plans. A plan to; feel good, not have to go near a hospital and not have to be in, manage my mood mode because something unexpected and unhelpful has triggered me.
Monday, you didn’t start out a bad day. In fact, you were brilliant until 6pm. I went for my morning blood test, at 8.30, later than usual after a wee welcomed sleep in and a fab, fun, friends packed day, on Sunday. Then, I moseyed to a café near hospital to do Italian language practice before my lesson with the fabulous C from Sardegna. I wandered back to Macmillan to a meeting with my therapist who helped me think about my recent test results, the meaning I was adding and my plans to up the ante on the work front. As usual she was a great help. My pink smoothie, a nutri-bulleted beetroot and green salad was yummy. My call with friend and coach M, was great. Even Chemo went smoothly. Or so I thought.
I got home and started feeling wretched. More wretched than I have in ages after a Chemo day. Even drinking water was difficult. Pain, everywhere. Nausea, constant. Stuck close to the bathroom. The Dom anti-nausea pill wasn’t doing its thing. Sweat, cold, sweat, cold. Aaargh. Why? Why today? This is sh*t. Will I function tomorrow? Hubby’s birthday is so important to me. He has even taken the day off work which is so rare. 10.15pm rolls around and Chemo you bit*h, you have me sitting on the couch, head in hands and between my knees.
Steroids

Then it dawns on me. I didn’t receive my steroids today. Dexamethasone, I wasn’t given it and I was so busy watching Americans on Prime to distract me from any pain of the cannula going in, that I didn’t do my own checks. Bugger. Now what. Now, I’ll have to telephone the Haematology Registrar on-call and see if I can take my day 16 (tomorrow’s dose) of Dex now. It’s not a great time of day to be taking a steroid, they’ll keep me up all night…but hopefully I’ll feel better. Priority right now: feel better.
Then I realise. Pissed off. If I take the dose I have at home, I’m going to have to go to hospital tomorrow now, the very day I didn’t want to go and normally don’t have to go near it. And on your birthday, darling Man. I don’t know how long it will take, to pick up a steroid on a day I am not usually there. VERY PISSED OFF. My feeling wretched, my having a problem, my having to go into problem solving mode, my having to deal with the impact, accept the consequences, pissed off…it was all so preventable. Annoyed. Sad.
I ring the hospital, ask for the Haematology Reg on call. Operator says she‘ll page him and he’ll call me back very soon, often straight away. I wait. 40 minutes later, I’m still waiting. I’m so sick, I can’t get angry. Hubby calls. The operator is surprised I haven’t heard. She pages him again. He calls back in 5 minutes. No apologies, no explanations (e.g on another call). He runs through the usual questions – have a vomited? Not yet. Do I have a temperature? No, just the sweat, cold combo. Do I have diarreah or constipation? No. Just pain, a lot of pain and nausea that pills don’t kick. Finally, he confirmed I should take the Dex I have at home and go up to hospital for another dose tomorrow.
I take the steroids and Hubby manages to find another stronger anti-nausea tablet amongst my large array of pills in ‘the pill box’ (a large bread bin, works a treat). I cuddle up to Hubby, focus on his breathing and wait for drugs to kick in. By the time we move it’s 1am and despite the steroid, I feel like my body is now desperate for sleep. Good. Happy to oblige. I drag myself upstairs to bed.

Hubby’s birthday day. I feel a whole heap better but very drained. He drives me to hospital. I go to get my steroid and my fear about how the day may unfold starts to be realised. Cancer, you bit*ch, you don’t make life easy. My steroid isn’t ready. I don’t get to drop in, collect it and get out again (my hope). Despite having an email back from my specialist in the morning, acknowledging that a) my Chemo, carfilzomib is hard to tolerate without the steroid and b) containing his request that I be dispensed the steroid today, directly from the Chemo Day Unit (CDU) and c) that the clinical trial nurse should call the CDU nurses to make sure they have the steroid ready for 9.30am – it’s not ready. I even get there about 10.40am, figuring I’d give everyone a bit more time to communicate and prepare.
I explain again, what has happened. The CDU nurses won’t give me the steroid and when they call the Clinical trial nurse for information something is lost in translation so they now think they need a prescription before they can give me anything. I show them my box of Dex with the prescription and dose details AGAIN. I start to get upset. Really upset. I could be waiting for ages for the clinical trial nurse to come to the CDU with a prescription (I’ve been through this before so know how long it can take) and then if I must go to the regular hospital pharmacy for it to be filled, I can write off another hour, it is hideously inefficient.
Tears. Yep they’re coming. I cry. M the wonderful receptionist comes to comfort me and says ‘this is not like you’ and to find out what’s going on. I fleetingly wonder ‘what is like me, when I’m here?’ I feel bad because I know the team have had someone die today and one of the head nurses has had to race off and manage that. My tears over impacting my day with my hubby seem trivial in comparison and yet not, nothing is trivial in this Cancer journey. It’s all bearable for me most of the time, yet it is all sh*t too. I cry some more.
Nurse L comes to my rescue. She looked after me all last year and I missed her when she left to do a stint in private practice. She asks what is going on, I tell her, show her my empty box of Dex and say I just need my day 16 dose because I had to take it last night after not receiving the steroids yesterday. I don’t say which Nurse forgot to give me the steroid. Nurses are human. We all make mistakes. She is usually so so good so must have had an ‘off day’. AND, it was my mistake too. It’s not really fair to hand all responsibility and agency of my care over to a Nurse. After all, I bang on about being the agent in your own health and treatment for as long as you possibly can. Nurse L goes and gets the Dex dose immediately and finally I get to leave.
Thank you M and L. You saved my day. I know my Clinician plans to talk to the nurses about how the steroid was missed but I don’t worry about that now. I know mistakes happen yet between us, the Nurses and I are usually so good at going through a checklist each time. It’s a shame it went wrong.
On this day of all days.
Psychology Tips – Working with your and others’ mistakes

Admitting mistakes can be hard. Research shows there are links between our beliefs about whether we can change our behaviour or whether our personality is fixed and if mistakes and admitting mistakes are perceived threats.1 Cognitive Scientist, Art Markman summarised the research results2 and explains when you believe that your behaviour can change, you are more likely to be willing to admit responsibility. You recognise that by admitting what you have done wrong, you can work to make it better, to grow and so you are not threatened or are less threatened by admitting mistakes.
People who do not believe that they can change, can be stressed by admitting their mistakes, because they believe that those mistakes say something fundamental about who they are as a person. Understanding that people see their own mistakes as a threat, and have different beliefs about their own and possibly others’ ability to change, can help us to remember to avoid showing unhelpful frustration and anger when managing mistakes. We can all change our behaviour. We can all learn from our mistakes. We can all repair and improve relationships. It can take some people longer than others, to recognise that change and growth is possible, especially when their starting point is one of: I and others have fixed personalities and mistakes are flaws.
It’s easy to get frustrated with others’ mistakes when we feel something is unfair (it can be completely justified) but does it help the situation to show the frustration? A compassionate response will get you more powerful results and responding with anger and frustration negatively impacts loyalty3,4. In my case, I want the Nurses to like treating me. I want them to feel we are on the same team, to feel loyal, committed. Showing my frustration and upset was normal, human, yet unlikely to have been the optimal way to have managed the situation. Remembering that frustration, anger and stress raise heart rates, make it harder to think, mean that when recognising frustration, a good first step is to pause, be mindful, and then choose a more powerful response. One of clear communication, compassion, kindness, empathy, forgiveness. This is more likely to invoke compassion, kindness and loyalty in return.
Recognise too that anger, frustration and upset at mistakes of yours and others are often underpinned and exacerbated by worry and a catastrophising thinking style. I was worrying that my need to go to hospital on Hubby’s birthday day would ruin our day. Ruin his day. Eventually I managed to realise an unhelpful worry and thinking style was probably in play and ask myself, was my hospital visit really the worst thing in the world? Were my thoughts true, would our day really be ruined? How much time in our day did it take up really? Was it more likely that hubby was happy to help and had enjoyed his rare time alone, in a café, doing things he wanted to do, without having to be at work, while I was at hospital? Regaining perspective enabled me to let my frustration and upset go. An hour later I noticed I was laughing at something Hubby said and our day was going well. Yes, it meant we came home earlier than expected because I was really tired yet we relaxed together and the evening was a good one. I could easily have been very tired anyway. It’s not unusual for the day after Chemo.

References:
1 Who accepts responsibility for their transgressions? Schumann, K and Dweck, CS. Who accepts responsibility for their transgressions? Pers Soc Psychol Bull. 2014 Dec;40(12):1598-610. doi: 10.1177/0146167214552789
2 Markman, A. (2014) What makes some of us own our mistakes and not others?
3 Sara B. Algoe & Jonathan Haidt (2009) Witnessing excellence in action: the ‘other-praising’ emotions of elevation, gratitude, and admiration, The Journal of Positive Psychology, 4:2, 105-127
4 See Adam Grant, Psychologist and author of Give and take: A revolutionary approach to success. See also work by Emma Seppala, Center for Compassion and Altruism Research and Education.
Acknowledgements:
Shadow and Dex pictures by Me
Dog Photo by Matthew Henry on Unsplash
Shattered plate Photo by chuttersnap on Unsplash
Failed it Photo by Estée Janssens on Unsplash
© 2018 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Chemotherapy for Myeloma, Myeloma Treatment, Psychology for Cancer, Symptoms and Side Effects Tagged with: Cancer, Carfilzomib, Compassion, Consequences, Dexamethazone, Frustration, Mindfulness, Mistake, Mistakes, Myeloma, Nausea, Psychology, Sick, Steroids, Sweats, Tears, Worry

February 22nd, 2018 by Janine
Dr L turned to his colleague and said, ‘for someone with Myeloma, Janine’s immune system is a Schwarzenegger’. Hey Arnie, you are now a metaphor for my health status. Who’d have thought?! It sounds so positive and I am very grateful that my precious physical self is coping so well with the toxicity of Chemo. I notice too that I get a little hung up on the ‘for someone with Myeloma’ phrase though more about that in the next post. Now, I want to talk about my relationship with my body. It has become a bit confused.

Can I share a secret? I liked it when cancer, chemo and a diet change caused me to lose weight. I like being closer to 60kg than 70kg. I like how slim and less pear shaped my legs look. I like being size 10 and for a few weeks, size 8. All my life, I have valued being slim, strived for it. I’m not obsessive. I don’t over exercise or starve myself or think about it constantly. Even when I put on two stone from IVF treatment: I hated it but didn’t panic. The weight had context. Once we stopped IVF treatments, I lost a stone quickly and then worked on chipping away at the rest. I like cake. I binge occasionally (or did before this new eating regime). Who doesn’t when there is a pack of dark chocolate hob nobs in the house and the hormones are taking over? I would say I’m weight and health conscious with no extremes.

I’ve never liked my arms: they’re too big. Well, apart from the time I sanded every spindle on a stair case by hand: my arms were toned, like Madonna’s or Geri Halliwell’s. I thought my arms looked great after that. It didn’t last long. Finding tops and elegant shirts to fit my arms has always been a hassle. The welcomed side effect from cancer, chemo and clean eating has been the slightly thinner arms and shirts fitting, for once. I don’t really want to give that up yet…
I find myself struggling. I’m in a tussle inside my head. Too much weight and muscle loss is not healthy, not helpful and goes against Dr L’s advice. He explained that he had noticed that people with Myeloma who keep up with the gym and have some muscle reserve seem to manage the chemo better. I do want to live as long and as well as I can. Yet I find myself loving my new size. I bought a pair of boyfriend jeans a few months into treatment, laughing with a wave of pleasure when I discovered I could fit into a size 10 only to find they slipped off a month later and I’d lost even more weight. Now what do I wear? Nothing in my wardrobe fits!!
At that point, 61kg, it did get a bit worrying. My face was looking drawn. My rib cage and spinal vertebrae were a too visible. I promised Dr L that I wouldn’t let my weight fall further. I expanded my food repertoire slightly (good quality bacon, goats cheese, sourdough toast occasionally) and started the weight training.

Back at the gym, I felt good and waves of relief from feeling stronger. I’d become so weak. I was asking hubby to open jars and water bottles for me and lift anything. This does not fit with my independent and equality philosophy. Yet, I dislike how quickly my leg and arm muscles grow. When my weight started to rise slowly I would find it hard to like what I saw in the mirror. I know it may seem silly in others’ minds. Intellectually, I know I look ‘normal’, ‘healthy’ and would still look heathy even if I did put on weight (I’m fortunate to be tall). Except, somehow it feels like a tug of war in my brain – Janine, don’t put on more bulk, you look good as you are (now size 10-12) versus Janine, you need more muscle and strength to manage Chemo effectively, get yourself to the gym.
For more years than I care to think about, I have gone to buy clothes and come back disillusioned when I have needed that elusive size 13 or 15. It seems crazy to have the same problem at a lower size (now 9 or 11) and with the added complication of my size constantly changing. I can’t afford and wouldn’t want to invest in new sets of clothing every few months yet as my weight goes up and down on chemo, what can I do? Frustrating. I hate being uncomfortable in clothes. I really dislike ill-fitting clothes that don’t help me feel good and enhance how I look in the world. Too loose is as bad as too tight!

Even more annoying, last summer, before diagnosis, I bought some new clothes after ‘making do’ for a few years. Now they are sitting in the wardrobe, barely used as they are far too big. I am in the maintenance phase of treatment, with 3 days rather than six days a month of Chemo and my weight is climbing and fast. I’m 67kg today. Maybe I’ll need those ‘larger’ clothes again in a couple of months. Except, I don’t really want to get any bigger or go back to the size of those clothes again. The 6 days of steroids each month may have something to say about that.
67kg. Nothing to worry about. Yet, I don’t feel good about it. I am beginning to worry that a steroid induced, sharp trajectory up of weight, will set in and hang around for the duration of treatment. There are 16 months to go! That’s a lot of weight gain. That makes me feel sick.
It is also motivating. I’m back on the high veg and protein regime. A few bits of non-clean eating crept in as I celebrated getting through the first 48 (see previous blog) and 9 months of treatment. Then I let the goodies stay, it was Christmas after all. Then I felt sorry for myself with the arrival of two viruses back to back. January came and went, and it’s always the toughest month in UK for me. It’s so often grey, cold, hibernation inducing and all I want to do is eat comfort food!
Oh well, not having the clothes I would like, in the bigger scheme of things, is insignificant really. If I hover around the 65kg mark and I am made of tiny Arnie style muscles, that will be good enough. Viruses and January blues are gone. The revolution is here. February has arrived.
I’m back on track with preventing my body from being a perfect host for cancer. I celebrate a new food focus: FISH. It is easy to do: I am languishing on the beautiful beaches of ANTIGUA for a much-needed holiday. Fresh snapper, mahi and octopus are on the menu. The company is great (hubby and besties), the sun is high, the sea is warm and the forecast is rosy. No time for weight tussles now: The bikini is out and about!
Acknowledgements:
Antigua seascape: Photo by me
Legs and kettle bell: Photo by Maria Fernanda Gonzalez on Unsplash
Clothes hangers: Photo by Christian Fregnan on Unsplash
Shirt and Jeans: Photo by Lyndsey Marie on Unsplash
Muscles: Photo by Alex Boyd on Unsplash
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Chemotherapy for Myeloma, Finance and Cost, Psychology for Cancer Tagged with: Cancer, Chemotherapy, clothes, muscles, Myeloma, weight
December 6th, 2017 by Janine
What a year! I turned 48, I was diagnosed with cancer and I’ve completed 48 chemo sessions. I love the number 48; it seems so symmetrical to me (I love a bit of symmetry). Now ‘48’ has a WHOLE new world of associations!
Warning…I have happy news, and, I’m going to talk about toilet rituals.
First, the rituals.
This may seem very strange to those of you who have always been super careful about hygiene when using public loos. In my defence, I have rarely worried about these things because my childhood in New Zealand was filled with non-traditional toilet arrangements. When you are fortunate enough to spend all day at the beach or walking in the bush or driving long stretches of deserted road or camping in remote sites you tend to get over yourself quite quickly about going to the loo wherever and however.
Doing your business quickly behind a tree, rock, or in a smelly long drop with minimal paper or alternatively leaves or seaweed, is not that unusual. Worrying about being seen was always a bit more bothersome than worrying about bugs, microbes or possible infections! The upshot is; I have never worried about using public loos, ‘catching anything’ or having to use disinfectant. I just focussed on washing my hands well.

Now that my immune system is compromised it’s another story completely….though maybe I’m being a bit anal? (pun intended)
In the Chemo Day Unit, patients are asked to ‘wipe the loo’ with anti-bacterial wipes before and after use. I recently discovered I had developed a wee ritual…Take a wipe, clean toilet seat, fold dirty side in, use clean side to wipe toilet handle, tap, hand wash dispenser, door lock, door handle. Dispose of wipe in bin. Use loo. Wash and dry hands properly – you know the 8-10 step process (depending on the poster). Take new wipe and clean toilet. Goodness knows what bugs I could pick up if I didn’t do this; don’t tell me!
Anyway, this is a new ritual in my life and once again one that seems to consume a little more of my available time and life though hopefully is worth it. It seems so, so far, as I have yet to pick up any major nasties despite lower immunity and chemotherapy for 9 months now. This ritual has now made its way out of the hospital and into public conveniences. AM I being anal? I’ll let you be the judge!


My News
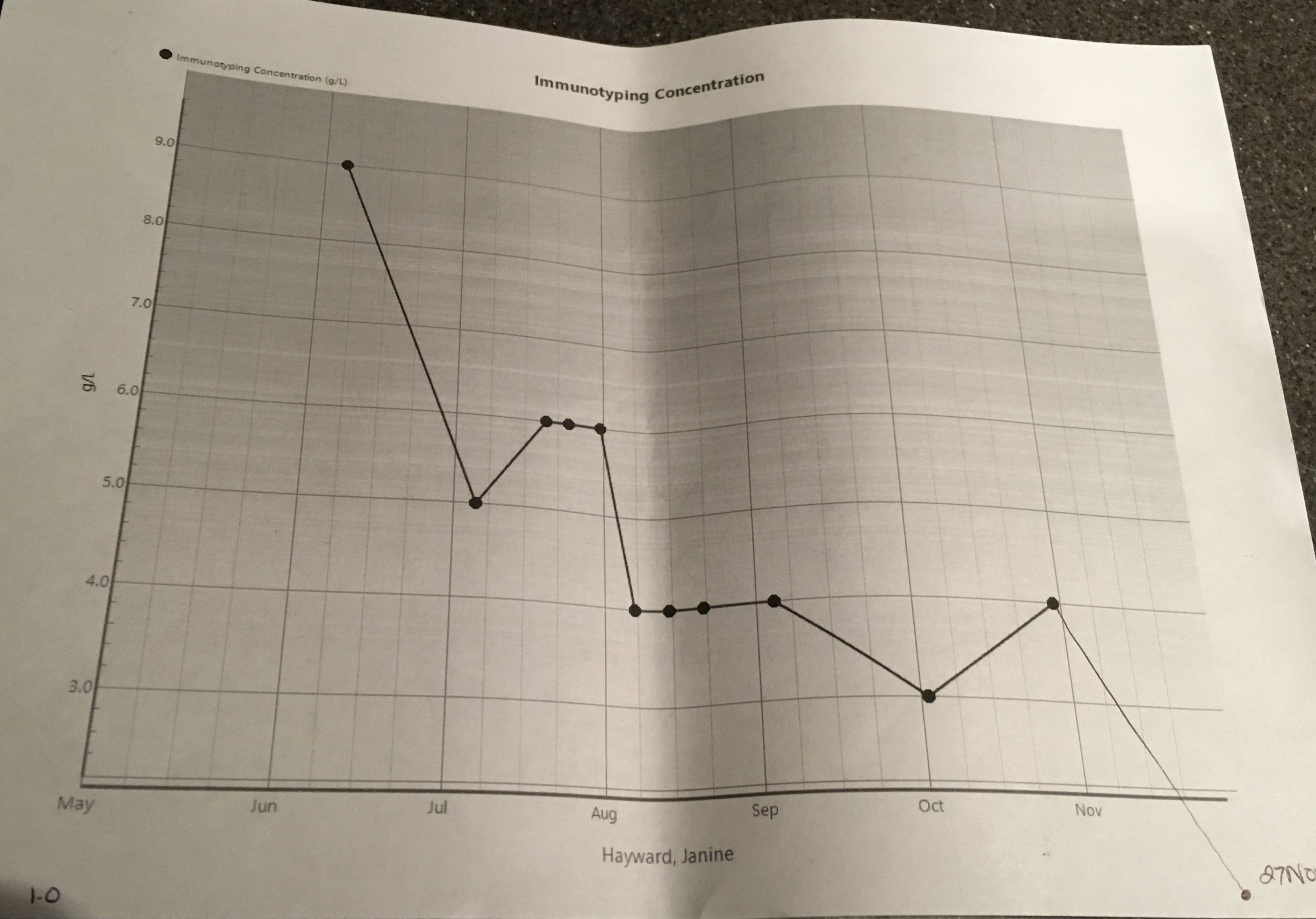
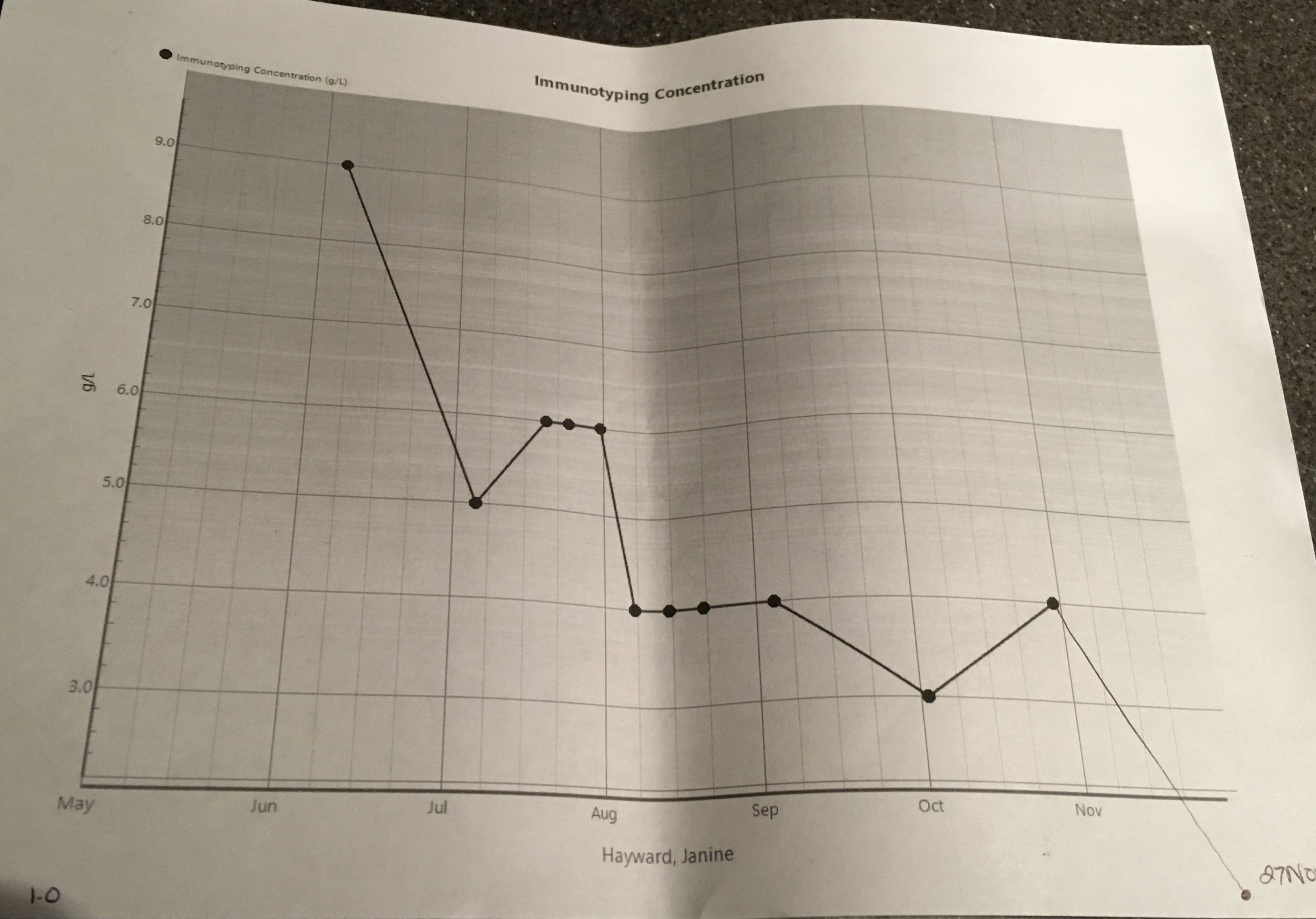
…is happy, positive and hope-FULL…I’m very grateful for it and its effect; a reaffirmation of my faith in my medical team, the drugs and my health and life choices. The Myeloma presence in my body has decreased further in the last few months… It’s down to 1 g/l (42 g/l at its peak) and a may be yet to plateau. Yee ha! Not only that, the serum kappa light chain results are 1.75 mg/l, backing up this great news and described as ‘excellent’ by Dr L. On top of that my liver is doing well. My Hb (Haemoglobin, the protein found in the red blood cells that carries oxygen around) level is back up to 121 g/l so I no longer need to consider taking EPO (yes, the cheaty cyclists’ drug of choice! I’m a tad disappointed. I had wanted to experience how energised I’d feel!) While 121 g/l is lower than the desired normal levels (125 g/l plus) it is great for someone with Myeloma. My kidneys are also doing OK for someone with Myeloma, my Creatinine is 69 umol/L and normal level for women is approx. 45 -90 umol/L (I think; there seems to be some debate!). Lots of good, great news, here. Dr L delivered these details and then reminded me to keep drinking 2-3 litres of water today for kidney care. I imagined my kidneys; bloated, water-logged, bean-shaped balloons, wrapped up in clouds of cotton wool, floating about, relaxed and without a worry in the world.


I’ve had yet another bone marrow biopsy and pet scan (what effect does three doses of radioactive sugar chasing gunk in a year have on one’s body? I guess I’ll find out!). I have an ear numbing full body MRI coming up in a fortnight.
Let’s hope they show (or don’t show lesions at all) that lesions are further dissolved and there are no new uninvited guests!!
What a year.
48.
One number I’ll never forget.
Acknowledgements
Images: Me (graphs va KCH), Long Drop – Sarang (public domain use permission granted)
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Chemotherapy for Myeloma, Myeloma Treatment, Results Tagged with: Bone Marrow Biopsy, Chemotherapy, Myeloma, Results, Tests, Treatment

October 31st, 2017 by Janine
OK Mr Tumour or more accurately Messrs Tumours. Listen up. Yep, all four of you. You know who you are. You are hanging around unwanted and uninvited. Where do you get off thinking its ok to be dossing about in my body? You’re a greedy bunch, aren’t you? Not contented with one spot, you hunker down in two places in my spine, my shoulder and my sternum. You threaten me with paralysis as you near my spinal cord and grow dark and big. What arrogance! Well, I have some words for you.
I have mindfulness and meditation and you are not going to like them. In fact, I already know you haven’t seen them coming. They have roughed you up a bit with their calm, kind, ease. Aww. Tough. If you can show up unannounced, I sure as hell can unleash mindfulness and meditation on you.
Your resistance is futile. You are already weaker. You can keep trying to hide out, munch on sugars (if I give you any) and try to take over the joint…but I know where you are. Your luck has run out. The Chemo is working. My new diet is working. My NHS medical team is great. I am doing fine. My mindfulness and meditation practice, reminds me this is so. Mindfulness and meditation practice, whether 5 minutes or 35 minutes; it’s getting to you, Mr Tumour (yes you, the large one in my lower spine). I’m talking to you.
YOU are DISSOLVING.
One at a time. Worst, darkest, nastiest first. You are dissolving. I know because I have seen you. My MRI showed me. You are thinner, lighter, dissolving, dying. Don’t feel bad. You are no match for kindness, curiosity, breath, acceptance, listening, powerful visualisation, practice of belief. Belief that my decisions about my treatment have been the right ones for me, that my medical team is the right one for me, the Chemo is the right Chemo for me and that I am doing fine.
My favourite guided meditation reminds me of this.
NOW you are DISSOLVING.
Meditation helps me visualise an all-powerful, protective, transformative, warm, healing light. It wraps up all four of you, Mr Tumour, you and your buddies, letting you know you are not needed. The light heals my body, generates new healthy cells, rids me of you. This same meditation helps me draw energy, power and peace from the Universe, imagine, believe and trust I am in safe hands, doing the best I can do. It is working. You are not running this show or in charge of this gig. I am; with the help and support of mindfulness and meditation.
Mindfulness for sleep. Mindfulness for Cancer. Mindfulness. It helps me to stop. To be. To breathe. To observe. Mindfulness, paying attention, moment to moment, in a kind, curious, non-judgemental way. Not like you, Tumours. You are random, cruel, unnecessary. Yet, thanks to Mindfulness, I accept you. I accept that you are here. I watch you, learn from you, ignore you and listen to you. I accept you have muscled your way in, demanded to be seen, to be heard. With Mindfulness, you don’t get to invade my every moment or even most moments. You don’t get to hurt my sense of who I am. You don’t get to take over. You get to be. Until, you are no longer being.
Listen up Mr Tumour. You are superfluous to requirements. While I accept you are there, I’m just letting you know you can go and take your friends with you. I know you are likely to return in the future; I’m a realist. Right now, you are not needed and not wanted. By the time, you want to make a comeback, I will be stronger than I am now, even more practiced in mindfulness and meditation, and healthier with years of a great low sugar diet behind me. I will have more chemo options and more effective medical solutions at my disposal. I will know more about you, your characteristics and the environment you need to thrive. I won’t provide it. You’ll have to find somewhere else to go or better yet not bother at all. I am ready now. I will be ready in the future.
I might have dark days and dark weeks through this journey Mr Tumour but that is nothing on how uncomfortable I am making things for you. I am not going to fight you. I’m not in a battle. I simply will not be providing the terrain that you want. I see you. You are dissolving. Soon I won’t see you. You are getter weaker. Myeloma may remain but you Mr Tumour are no match for my healing light. You do not have to stick around. Mindfulness and meditation, they’ll remind me why you came and what you can teach me. I won’t forget you. I don’t however, need you. I will watch you dissolve. You can leave now. Thank you.
Three of my favourites;
Meditation
Survive Thrive and “Dawning of the Day” by Aine Minogue
https://youtu.be/MNaqEKtc4Uk?list=PL2a9c2CFCJdlYehE9jochHrjWFMq4AHiu
Mindfulness
https://www.headspace.com
http://franticworld.com/resources/free-meditations-from-mindfulness-for-health/
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Chemotherapy for Myeloma, Psychology for Cancer Tagged with: Cancer, Dissolve, meditation, Mindfulness, Myeloma, Nutrition, spine, Tumour
July 19th, 2017 by Janine
I’m going to be sick. I’m running to the bathroom. I’m not going to make it. I’m scanning for basins and thinking use the kitchen if I can’t make it to the bathroom. At least make it to the tiles, it will be easier to clean up. I make it, this time. While I’m trying to keep my hair out of the toilet bowl and not notice how sore my knees are on the floor I start thinking; Where did this nausea come from? The last three months have been relatively easy; is this what Chemo is really like? Is this the nausea others talk about? Well they can have it back; it’s awful. And it’s not the worst thing.
I slowly make it back to the couch and lie down. I’m wondering if this last month of induction treatment is worse because I have responded so well to Chemotherapy over the last few months, now there is less cancer to vamoose; more good cells are copping it. I’m thinking about this when I notice my brain is getting hot. Not my head, not like a headache; my brain. In fact, its not just hot, it’s getting hotter by the second. My brain is on fire and I’m not sure I can cope. My eyes feel heavy…and hot. I can’t keep them open but I feel sick and am going to have to get up any second to go to the bathroom again. At this rate I’m going to need a couch near the bathroom or in it, not that it would fit. My brain hell fire is getting worse and my body is screaming at me to close my eyes, sleep, now!
I can’t, I have to go back to the bathroom. Ginger tea isn’t working this time. The anti-nausea pill isn’t working either. This chemo experience is different, and besides, I can’t keep anything down. So much for gaining weight or staying hydrated. A bit hard to do when I’m vomiting. I manage the journey to the bathroom, throw up and hang out for a while waiting for the next wave of nausea. I have a picture of my brain burning bright yellow and red with solar flare flames coming off the top of it, searing their way out of my skull. My brain feels like it is about to explode. It’s excruciating. Am I literally being fried with chemicals? I make it back to the couch and succumb gratefully to sleep.
From 4pm to 2am I’m in the bathroom or asleep. When I wake I feel trashed, tired but better. I eat two rice cakes and marmite (love it or hate it, it has its moments) and manage to take my meds. Relief. I feel slightly normal again. I watch TV for an hour and go upstairs to bed.
Sleep has been elusive over the last three to six months. I often wake every 1-2 hours. I am feeling a bit low and constantly tired despite the steroids. Unsurprising really when I’m not sleeping well. I talk to Dr L about pills and the nausea/brain fire. He takes control and agrees sleeping pills are a good idea and proposes a second anti-nausea drug. He doesn’t want me ‘putting up with’ anything. Relief again. I am finally going to get a good night’s sleep. Florence pops into my mind.
Music; Dog Days are Over, Florence and the Machine
For the first three months/rounds of Chemo I’d had no anti-nausea help and found using simple ginger tea worked. Now, I’m using two lots of anti nausea meds and ginger tea. The pfaffy thing; I need to remember to take the new meds 30-60 mins before food, three times a day. More stuff to think about when there are already so many pills and supplements to keep a handle on and information about upcoming treatment to process. Still, I’m highly motivated to prevent “brain on fire” and vomiting every five minutes – funny that.
The flag at Kings College Hospital is at half mast during my hospital visit, appropriately, for the victims of the horrendous attacks in London and Manchester. I feel strange too; grateful for not being in one of my favourite areas of London, an old stomping ground, at the time the attacker was there and yet also wondering how I would have reacted if it was me the person with a knife had come after. Does knowing you are dying sooner than expected change how you might react in crisis? Would I have run or taken more risks? Thrown things at the attackers, tried to fight back or help those that had been stabbed? Who knows? I can’t know. I’m grateful in many ways for not knowing and yet I’m curious about whether I would be different now.
The rest of month four passes without too many glitches and the best thing is getting some sleep – hurrah! I’m a bit depressed about how much strength I’ve lost though, and how old I feel when I can’t undo a jar lid or carry something I’d usually be able to carry. Weight training is now 20 reps of 1kg weights rather than three sets of 12 reps of a much higher weight. Fatigue is ever present.
This is not a novel new project anymore. The chemo, the eating regime, I’m over it. I want a break.
Editorial Support: Stephanie Kemp
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Chemotherapy for Myeloma, Myeloma Treatment, Symptoms and Side Effects Tagged with: Brain, Cancer, Fire, Myeloma, Nausea, Sick, Side effects
I bopped down the hospital corridor towards the Chemo Unit (listening to a bit of Adele) and started thinking back over this cycle of treatment. It’s not a good or bad news story. It’s a GREAT news story. Yes, there are a few side lines about niggly things, just to keep it real. Great news though; we can always do with a bit of that, can’t we?
Music – Music was back, yay! All a bit eclectic, and hey, that’s how I roll!
The theme-tune from Cheers: Where Everybody Knows Your Name, Gary Portnoy; On the Level, Mac DeMarco (calming and grating at same time); The Only Way Is Up, Yazz; Rapture, Blondie; An hour of Radio 1 in an afternoon; Right as Rain, Adele (transpose talk of lover with Myeloma; it works!)
Also gobbled up podcast S-Town, Serial Series 2 (Series 1 was great too).

Medical Update
Here’s a graph. I love a good graph, don’t you? I especially love this one as it shows some important stuff going in a mighty good direction. Cancer presence is trending down. My chemo response rate is trending up! Yeah, baby!!! I’m not fighting with Myeloma; I am guiding it to the door, hoping ultimately to close the door behind it for as long as possible.
The great news
My para-protein level, the indicator of those unwanted Myeloma plasma cells (now kicked to dust over the first two cycles of Chemo) is looking good, very good. My results have come down: from 40 g/l at diagnosis, up at 42 g/l when starting treatment, down to 17g/l by the early part of this cycle and by the third week, 11 g/l. The medical team look for (and the clinical trial requires for next step progression) a minimum of partial response (PR) by the end of the induction treatment (four cycles of Chemo). PR is a drop of 50% of presence of Myeloma indicated initially by the para protein level. The good news is that I had achieved PR by the end of Cycle Two! Also, the para protein level has kept heading in the right direction: down! I still have one cycle to go in this round so a great overall response rate seems so possible right now. And I am still gunning for 100%. I hope I am not too disappointed if 100% is not achieved.
The niggly things

It was a tough start to Cycle Three. I was feeling a bit low. On day one, Si and I attended a clinic appointment with my Clinical Trial lead. It was helpful, and he kicked off the conversation about the stem cell harvest. It was also awful. He went over the prognosis again: the incurable nature of Myeloma. Then he followed with the dramatic strides that have been made in the last two years with new drugs and better outcomes. They are better outcomes: people with Myeloma receiving treatment used to get three years, recently they were getting seven, and now the average is 8-10 years. Great strides, but still short, and I had trouble on that day hearing it all again. I wanted to focus on next steps in the treatment instead, not how long it may or may not ‘get’ me. I left feeling utterly drained and not overly well-informed about the cell collection as I had trouble listening to these points with loads of the other stuff in my mind creating noise.

While the scaredy needles seemed to get over their fear this month (Nurse L worked her magic), a strange rash appeared down my left arm (worse than the little bit I had experienced in early days of Chemo) and it hung about for a couple of days. No known cause at this stage and something to look out for again. My calcium level dropped a bit so I now take calcium tablets too. My urea and creatinine levels dropped for a week. These returned to normal after I focussed on keeping up the three litres of water a day and recognised night sweats might be dehydrating me a bit more than I had thought.
Long waits for Chemo occurred on a few days. One day was over three hours and down to a process issue; these kind of things happen sometimes yet are usually preventable. I gave what I hope was constructive and gentle feedback to the medical team. They were supportive, listened really well and agreed a plan of action. A Clinical Trial Nurse, M, thanked me for being an active partner in my treatment: for my feedback and follow up on things they have mentioned in the past, such as providing patient diaries and requesting new ones if they have not been received. Her comment felt genuine and I really appreciated it. I never want to overstep or cause additional work, yet my nose for process re-engineering and efficiency often rears its head, especially in the NHS. The NHS is awesome (free!) and could benefit from regular process review, especially as when used well, reviews and service/process development ultimately save time and cost. Hey, who has time to do timely reviews? More appropriate NHS resources required! Let’s hope Brexit doesn’t scupper that. Or the upcoming election.
Other great things; small and large
I attended a helpful webinar through MMRF that shared the latest USA understanding and treatments. Lots of promising diagnosis tools and new drugs are coming down the line that will hopefully be available in the UK by the time I need them, after my initial remission period lapses. I also attended a fabulous day at Kings College Hospital where the latest UK-based clinical trial information and outcomes were shared. We were given a tour of the labs in which blood and marrow are analysed, stored (at -196 degrees) and the clinical research facility. After donning the blue plastic shoes, hair bands and protectors to ensure we didn’t cause any contamination, we were taken into one part of the facility where we could safely view the highly-restricted areas and complex equipment – very ‘CSI’ (for anyone who has watched those TV programmes as much as I have). We learned about how contamination is monitored and prevented, and how studies of highly sensitive blood and organs are undertaken. Fascinating, and a real privilege to see ‘behind the scenes’ in this way.
My girlfriend B came along to Chemo with me on day 2 this month and it was so great to have her there. She was calm in a strange environment and we laughed together which was fab. Strangely, despite the circumstances, this day and another day on which we did meditation together and a third day when we made time for a great lunch date (unfortunately just before she left London; would have been great to fit in more of these) really stood out to me as special moments, quality time and very supportive.

We finally christened the table tennis table (Si’s birthday present). I am queen of the table; the presiding champion in the round robin between Si, my brother-in-law and me. Of course, were you ever in any doubt? Si didn’t like that and brought up other stories about me beating him at clay-pigeon shooting over ten years ago during another birthday present experience for him. Ooops! Although, wait until Mum gets here, she tends to claim table tennis crowns!

On the last day of Chemo this month, I wore a dress and two people told me I looked lovely. What a great start to the day. Especially as I felt very tired that morning. Choices again. I could have worn tracky bottoms and a top like I did the day before and that would have been fine. I needed a pick-me-up. A dress and makeup was a helpful move. After all, I felt better. It was great to dance in on the way up to Hospital, feeling the fabric move around my bod. And hey, it resulted in compliments – the dress, not the dancing! Worth it, that little bit of effort. I might not have the energy to do this next time and that’s ok. It was lovely to grab the moment on that day.
Thank you
Thank you to you, the readers; there are now over 800 users on the Psyching Out Cancer blog.
Psychology – Reflection
Life is a daily, weekly, yearly roller-coaster of good, difficult and neutral events that come and go. Our response to each event – small or huge, the attention we give each, the meaning we add, the willingness to accept the unchangeable – all dictate how we well we cope with the rollercoaster. Our ability to pause, notice, and choose a response, facilitates how much we stop and enjoy the good times, and ensures the more difficult times have less impact on our day to day lives and long term goals. Sometimes though, we forget to pause or find it difficult to pause; this is where in addition to knowing our triggers for unpleasant reactions, Reflection is crucial.
Reflection is defined as serious thought or consideration. In psychology, reflection often involves a therapist reading or saying the client’s words back to the client so that they can hear for themselves what they have said and evaluate the logic or reasoning behind their own statements. You can also be your own therapist with reflection. Self-reflection can be referred to as examination and contemplation of our own thoughts and behaviour; helping ourselves to hear and evaluate.1-3
There can be no knowledge without emotion. We may be aware of a truth, yet until we have felt its force, it is not ours. To the cognition of the brain must be added the experience of the soul.
Arnold Bennett (1867–1931) 4
The lessons I have learned, and psychology skills I have applied, this month have often been difficult to remember to use in a timely manner and I have needed time to notice and understand my reaction and needs. The post reflection lessons have been transformative and confronting; they have led to open, honest debate with myself and communication with others such as in my previous post ‘Killing Me with Kindness’.
All in the Mind, a BBC Radio show presented by Claudia Hammond, is a fabulous resource for learning about mental health (links below). The show often hears from people with experience of mental health difficulties, charities working in this space, expert clinicians, and academics and researchers who explain the latest evidence about incidence and treatment, and debunk myths. In one of the recent episodes, evidence was presented about the power of expressive writing about your experiences and the positive outcomes that were experienced.
Writing can be, for some, a great way to facilitate reflection. Whether it is keeping a diary, or writing a letter to yourself or another, writing about how events made you feel emotionally and physically, the thoughts you noticed, what you were curious about or wondered about in terms of the event, yourself, the other person’s thinking, feelings, reaction, motivations. It can be so helpful to ‘not to make the person wrong’. Instead, focus on the event or behaviour and how it made you feel, how you thought it might have made the other person feel, with curiosity and compassion. Recognise that you may have their feelings and thoughts wrong; be careful not to assume and instead be curious. You do NOT have to send the letter. You do NOT have to keep the letter once it is written, though you may find it helpful to send or re-read them; only you can decide this.
For those that don’t like writing, a Dictaphone, a voice recorder, or even an app that converts your voice to word or pages can be used.
If neither of these appeals, taking time out simply to be and think about a past event, day, week, a particular period, can be useful. Notice all those things above, and also notice what worked well, what worked less well, and what you would do differently or not do differently.
Alternatively, and I highly recommend this approach (which can be done alone or in combination with the others above) solely focus on taking time to sit, put yourself back into the event and be with whichever emotions, light or strong, arise. Allow yourself to feel them, deeply, outwardly with tears, or anger or another response, if that is what arises, without judgement of yourself or anyone else. This type of reflection helps your body and mind to fully experience and process events together. Regular reflection, not rumination where negative thoughts are given repeated attention, but regular curiosity-based reflection, can help process strong emotions.
All regular reflection can help your mind and body notice when similar events are happening again, often earlier than usual, and sometimes even in the moment. This observation then allows for pause and choice of response; helpful or unhelpful, one that serves you well or doesn’t serve you well.
Remember, after reflection, be kind to yourself; your responses and emotions within reflection are normal. If you feel upset or angry afterwards, take 5 minutes or more to do something enjoyable even for a few minutes; take a few deep slow breaths; tell yourself you are ok, safe, good enough; read a magazine; do one yoga sun salutation; make a cup of coffee; close your eyes; do a body relaxation exercise, a tai chi movement, a back stretch or something else relaxing and fun to bring your arousal level down before trying to get on with your day.
Summary
Reflection is an important skill for maintaining good mental health and one worth investing time in practicing: through writing, dictating or focussing on your experience in a curious way that allows you to fully experience your emotions.
Great News
Cycle Three – done. A roller-coaster and many highlights of great news. Onwards with Cycle Four, the last month of Chemo before the next phase of treatment. Gosh, the time has gone quickly.
Resources
BBC – All in the Mind. http://www.bbc.co.uk/programmes/b006qxx9
All In The Mind, Episode including benefits of expressive writing (15 May 17) http://www.bbc.co.uk/programmes/b08n2wcz
Gibbs Reflective Cycle (in Dye, 2011), University of Cumbria (2016)
http://my.cumbria.ac.uk/Public/LISS/Documents/skillsatcumbria/ReflectiveCycleGibbs.pdf
Acknowledgements
1 Oxford Dictionaries https://en.oxforddictionaries.com/definition/reflection
2 Alley Dog Psychology Glossary https://www.alleydog.com/glossary/definition.php?term=Reflection
3 Psychology Dictionary http://psychologydictionary.org/self-reflection/
4 A return to the use of emotion and reflection. Helen Demetriou and Elaine Wilson
https://thepsychologist.bps.org.uk/volume-21/edition-11/return-use-emotion-and-reflection
Images: B, Me
Editorial Support: Stephanie Kemp
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Chemotherapy for Myeloma, Myeloma Treatment Tagged with: Cancer, Myeloma, Para Protein, Partial Response, Psychology, Reflection, Response Rate, Survival Rates
It’s been hard to write the blog in week’s four, five and six of Chemo; I didn’t know where to start, there didn’t seem to be time, and I was worrying. Even Music didn’t show up much; I didn’t hear it or go looking for it – strange.

I started to worry about having little time; not time on this earth but time during the day to do all the things I needed to do. Sound familiar? I have learned over the years that when I worry about not having enough time, it usually means I am probably trying to do too much and am not getting enough rest or chill space. I noticed too that when reminders popped up in my calendar to get some ‘headspace’ or do a visualisation, I was swiping them away and thinking I’ll do that later yet later never came. This worried me.
I wondered whether my blood test results for week four would not be as good as the previous weeks and imply that going away to Canada had been a bad call after all. It turned out this worry, while natural, was unfounded; my results showed more test results falling within the normal range than in the previous weeks and suggested my immune system was hanging in there – a good result.
I worried about an interaction with a Nurse and found myself feeling ‘told off’, then wondering if I was being over sensitive, or not sensitive enough to others. I felt guilty for coping well with and doing well on Chemo. The nurse had asked how I was doing and I had said something along the lines of “really well thanks” and “chemo had been quick today”. I heard a response of “well that’s not the case for everyone”.
Then a stream of thoughts flooded my mind;
- Sh*t, had I spoken too loudly?
- A lot of people look very ill and drained on the Chemo ward today, have I not thought of them? Should I think of them?
- I have answered honestly and positively; that’s what I committed to do throughout this process wherever possible.
Feeling a bit indignant, more thoughts rushed in;
- No, it’s fine for me to be positive after all it’s not my fault I’m doing well,
- Being positive is meant to help with healing so I’m not going to stop answering ‘I’m Doing Well’, when I am doing well.
Overnight and with reflection I decided I probably was being a bit sensitive and it was also fine to be positive. The following day I checked in with the nurse, who quickly reassured me that he had not thought I’d been insensitive to others on the ward at all. We cleared any misunderstanding and he reiterated how great it was that I was doing well. This frank discussion helped bring clarity and perspective to my thoughts. It stopped this worry completely. I’m glad I raised it with the nurse even though I was uncertain (and nervous) about what I might hear.

Despite this resolution, a residual sense of stress, worry and an over active adrenal system remained; the opposite of the many calm moments that I had been experiencing last month. The overall worrying continued.
My weight had dropped again to 66kg and I was struggling to eat enough calories. I often didn’t feel hungry but still tried to eat. I hoped my weight would stabilise and even climb back up to 68kg. That weight had felt comfortable while now I noticed I didn’t seem to have much padding, wondered if I really did have much of a reserve if I got an infection and I noticed I had lost muscle mass. The backs of my hands look like some very elderly person’s hands; dry and wrinkly despite the constant fluid intake. I worried that my weight would keep falling and my skin would get worse.
I worried about whether I should stick to the plan of not working for six months to focus on getting to remission as successfully as possible or to work while I still could. I worried about if I worked, would it be too stressful, leave me enough time to rest or feel like it’s getting in the way. I worried about not being able to work out how much work was too much, and for private practice whether enough work matched with breaking even financially. I worried about how to contain my clients’ concerns if my appearance changed with more chemo and how I provide a consistency of safe space for them if my medical appointments needed to change in the future. I worried and yet I missed making a difference and being the psychologist I know I can be.
To cap off the week, I finally had a long-awaited Ear, Nose and Throat appointment (yet another hospital visit) to check my possible hearing loss. This is something else I have been worried about for a long time and that has no doubt been bugging Si for years as I constantly ask him to repeat himself or need the TV volume well above the level he would choose. I had noticed my hearing was worse when; I’d find it difficult in crowded places (and with background noise) to hear the person I was standing next to and speaking with, or to hear what someone was saying if I couldn’t see their face and mouth. I noticed I had started guessing (not always accurately) what someone was saying.
For a psychologist; listening skills are imperative and before listening skills can be invoked one has to be able to hear! While I had rarely experienced these problems in one to one therapy sessions, I was concerned symptoms would get worse or impact my functioning. Sure enough I wasn’t dreaming this either; tests showed my hearing has deteriorated though is still in the mild loss range; inner ear cochlear deterioration so unrecoverable. This is essentially the kind of loss most people start experiencing from around 60 years old on…except I’m not 50 yet! I suspect I’m paying the price for good times; a burst ear drum while scuba diving as a teenager and damage from standing far too close to speakers at Fabric nightclub a few years back (ok, so quite a few years ago now).
So I’ve been worrying and it’s completely natural to worry. It is not helpful to dwell in worry or worry about things I can’t control so how do I let go of it? Worry is something I have helped many clients with over the last ten years so it is definitely time for some self-help. Below are the psychology tips and strategies I reminded myself to use.
Psychology – Overcoming and managing worry

What is Worry? How worry works.
Worry is a form of mental problem solving about potentially negative future events. It can be triggered by a variety of external events or from thoughts that just pop into your head. Worry is characterised by a lot of ‘what if’ questions. For example, ‘What if my Chemo doesn’t work?’ ‘What if my new boss doesn’t like me or think I’m good enough?’
Normal worry is usually short lived and leads to positive problem solving activities. Worry becomes unhelpful when it is about several things, is frequent and difficult to control or dismiss. We can think prolonged or frequent worry helps with problem solving, planning and preparation however worry breeds more worry (and anxiety) which prevents positive thinking and action.
Worrying can rob people of time. It’s exhausting and often leaves people feeling tense, with disturbed sleep, difficulties concentrating, and feeling irritable. While sometimes it can feel appropriate or necessary, worrying is exactly the opposite; it’s restrictive, and takes up time, attention and energy that could be spent on useful, enjoyable and meaningful activities.
Why do some people seem to worry more than others?
Worrying is human! The causes of are not clearly understood though it may be that a number of vulnerabilities increase the chance of developing a tendency to worry excessively; prolonged stress, past experiences of uncontrollable or traumatic events, an inherited biological disposition to experience negative emotions, learned messages from others that the world is unsafe or that worry is useful, and a coping style that involves avoiding challenges or situations where there is a chance of experiencing negative emotions (which prevents positive experience of coping and positive emotions).
Managing worry.
UNDERSTAND YOUR WORRY CYCLES – Understand your vicious cycles of anxiety and how avoidance contributes to anxiety. See the handout below (CCI – Vicious Cycle of Anxiety).
NOTICE YOUR PAYOFFS AND COSTS. Part of understanding your worry can be to notice if you are getting a pay-off from worrying, ‘buying into it’ and most importantly what the cost of the pay-off might be. Are you avoiding going out? You might get a pay-off of avoiding any negative emotions such as uncertainty of what will happen or be said when you see someone but you also miss out on the potential positive experiences; fun, laughter, connectedness or ease which going out may also provide. Also notice, where do you worry and what are you doing when you worry. For example, are you sitting down and telling yourself ‘you are worrying but getting rest at the same time’. Consider that your type of ‘sitting down’ in this instance is not truly restful and what it actually costs you is feeling rested. If you shifted your attention away from worry to giving yourself permission for genuine rest, and allowed yourself to do something enjoyable without the worrying in that same time, you are much more likely to feel rested and relaxed (and be better able to cope with normal levels of worry that we all experience).
Other practical strategies:
USE A WORRY TREE to identify where to put your attention so that you shift your attention to worries you can do something about and form a plan for rather than worries you have no control over. There is a link to a handout below
CHANGE “WHAT IF’ STATEMENTS TO ‘HOW’ STATEMENTS’. For example, instead of “what if Chemo doesn’t work?’ I might ask myself ‘How will I act if Chemo doesn’t work? How will I find out what action can be taken next?’
POSTPONE WORRY. This is where you give yourself permission to worry about a specific topic, at a particularly time later in the day, for a maximum duration of say 20 minutes). This way you are acknowledging your concern and allowing yourself to think about it for a contained amount of time without it taking over and impacting the rest of your day. Sometimes you may find the thing you were worrying about has resolved itself by the time the allotted worrying time has come around, or it looks completely different and isn’t as big of an issue as it seemed earlier or doesn’t have to be dealt with today after all.
Summary
These are just some tips for managing worry and there are others if these don’t work for you. Remember, while worry is normal, excessive worry can be gripping and creep up on anyone. Even when worry can feel like a good thing to do, it creates more anxiety. When it stops you from enjoying life or doing the things you want to do, worry is not your friend. Excessive worry can be overcome. Please try the strategies outlined above and the links to helpful handouts below. If you find them hard to do alone, do talk with your GP or ask a psychologist to help with gaining treatment or to work through the strategies with you.
Acknowledgements, Permissions and Helpful Handouts:
Centre for Clinical Interventions (CCI), Department of Health, Australia http://www.cci.health.wa.gov.au/
CCI Generalised Anxiety and Worry
http://www.cci.health.wa.gov.au/resources/infopax_doc.cfm?Mini_ID=46
CCI Vicious Cycle of Anxiety
http://www.cci.health.wa.gov.au/resources/docs/Info-Vicious%20Cycle%20of%20Anxiety.pdf
CCI Postponing Worry
http://www.cci.health.wa.gov.au/docs/ACF3D66.pdf
Get Self Help Get.gg – Worry Tree
https://www.getselfhelp.co.uk/docs/worrytree.pdf
Images: Simon Hayward
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Chemotherapy for Myeloma, Psychology for Cancer Tagged with: Cancer, Chemotherapy, Myeloma, Psychology, Worry