It may not be very British but I’m going to talk about money. When this Myeloma journey started, my hubby and I immediately obsessed and worried about money, about what a cancer diagnosis could do to us, and how much treatment would cost. I was disappointed, ashamed and annoyed to discover my NZ life term insurance had recently expired. It had always been a comfort to me that if anything had happened to me, Mum and Dad would get some money which would at least cover any unforeseen expenses such as Mum and Dad coming over for a funeral, funeral costs etc…but no, I let it expire without reviewing it….and the NZ insurance company who had happily taken my money each year had failed to update their systems with my new contact details, ensuring I didn’t receive any notifications of impending expiry. They don’t offer that type of insurance anymore and so to renew, instead of paying an affordable sum, I would have to pay upwards of six times the amount for less coverage, and the fee would increase annually. This would only be an option, of course, if I could get past the health questionnaire. Here’s the first thing, that turned out to be costly.
Next, and we put our hands up, it was our fault, after having health insurance for over ten years, we had just gained quotes for renewal and then decided to defer paying for a new policy for a few months. We surmised, incorrectly, that we were fit and healthy; it could wait until hubby had changed job as health insurance often came in the salary package. If he hadn’t secured the job he wanted within three months, we would take out a separate policy. Murphy’s law, cancer turned up in our lives, within the first month of the period with no cover. We felt embarrassed, upset and kicked ourselves that we had taken this risk; it hit hubby hard. He felt guilt and worry that he may not be able to provide me the treatment and care experience that he wanted for me, without private health insurance options. That wasn’t necessarily the case but we didn’t know that at the time; he felt awful.
I was worried about money and treatment experience, and I knew, we had made the health insurance deferral decision for what seemed the right reason and sound risk assessment at the time; it was, what it was. There was no point worrying about it now. As it turned out, with all things weighed up (including the cost of self-funding; a minimum of £15,000 per month for approximately two years and that did not include stem cell harvest and transplant procedures), I more than likely would have chosen the NHS trial route anyway (or maybe this is choice bias at work?!) and so this decision would have had minimal impact.
The hidden cost, has turned up when I have tried to get health insurance post diagnosis (you know, for all the things that can happen to me health wise that are not about cancer); not a simple or affordable task by any means. If you have had or are living with cancer, many insurers simply won’t insure you. Too bad, if I get hit by a car crossing the road and break my leg (nothing to do with cancer). This is yet to be resolved. Thank goodness, the NHS is usually fab in emergencies.
More costs turned up, and this was all before getting to day to day living costs that seemed to have quadrupled since cancer arrived. I had just finished a doctorate and as many readers now know, we had planned the trip of a life time with friends to meet in Canada for skiing. A wonderful luxury, saved for and highly anticipated; a fitting reward for all our hard graft over the previous five years. First our flights had to be changed and a new flight purchased, some accommodation and car rental costs forfeited and new ones incurred all to ensure I was back in time for treatment. Next the company we had paid for travel insurance with, over the previous 15 years and with whom I had never claimed, cancelled our policy on hearing of my diagnosis – not just my policy but hubby’s as well!
Trying to find travel insurance when you are newly diagnosed with cancer is not easy. Only a few insurers do it, they ask a whole heap of very personal questions (that I had never anticipated having to answer) but that is not the kicker. The kicker is that instead of paying £120 for a comprehensive travel policy that includes all the sports, the cheapest policy I could find was well over five times as much and gave me considerably less cover. Nice! A real, kick you when you are down, moment. For a few minutes, to myself, I cried and threw my toys out of the pram; how dare they? Don’t they know this situation is hard enough? My holiday has been spoilt. I’ve got cancer! They’re exploiting me. They know I don’t have a choice but to pay their charge or not go on holiday, how cruel can they be? Bast***ds’. Why was I being kicked while down and discriminated against? Obviously, I am not meant to travel when I am living with cancer or recovering, I am contaminated and meant to stay at home, rest and be quiet. Expensive, that’s what it is. I felt hurt and upset. Apart from the cancer, I was well, managing my treatment well and doing everything I could to ensure I would not need to go to hospital or need any extra meds while away (hell, I was even away with a medical expert) yet I was still required to pay a crazy amount for travel insurance. In the end, I paid, putting quality of life over money. I know I was lucky to be able to do this (see post Elk-ibou on the corner of Fox and Cougar).
Health insurance is expensive and hard to get. Travel insurance is expensive and hard to get. What next? Everything. Living with cancer, everything has seemed more expensive. If it hasn’t cost extra, it has usually meant I have had to trade off not incurring an expense with doing/buying something that may be helpful or healthier for me. The books I’ve bought about Cancer and how to survive; the organic food, supplements, the nutrition appointments all to ensure I was doing the best I could do for my body; weekends away that I booked because I worried I would become too ill to travel, anywhere; the glass containers I bought which were ‘safer’ than the plastic we’d lived with for years, the cleaning products I bought to eventually swap out with the brands I was used to buying, the bees wrap instead of cling film, the natural instead of usual skin care, all to avoid harmful toxins, parabens, BPAs and the like; the nutri-bullet and extra cups for the plant food smoothies, the non-dairy milks that are more expensive than milk because I’ve been advised to avoid dairy food for a while; the new clothes, I didn’t want to waste money on but had to buy because my clothes were dropping off my new plant food/chemo’d1 frame; the new, old car (plus insurance, MOT, resident parking permit) that we bought in case I became too ill to get to hospital appointments but had been managing perfectly well without, ‘before cancer’…these have all been costs we would not have had this year or ever, if I hadn’t received my news of Myeloma. If I keep thinking about this topic, there are other costs too but I’ll stop here before this list becomes overwhelming.
Many of these costs may appear non-essential; if there is limited income and children to feed and support, I understand how many people living with cancer may not spend or even have the money to spend on books, blenders and the like. And there it is…the big question, how much does the ability to afford these changes, impact outcomes of; overcoming cancer, managing treatment or at the very least, living the highest quality of life possible?
What a horrible situation to be in, a horrible choice to have to make (if there is a choice, and for a parent particularly); asking themselves, do I spend the money on things that may help me overcome cancer or stay as well as possible, for as long as possible or do I forgo those expenses because we don’t have the money for them or because I don’t want to spend the money spent on me, when there are kids to provide for? In my case, with no kids to consider, I found myself also thinking, I don’t want to waste money because Si still has a life to lead after I’m gone. We have built our assets together so why should we spend all the assets we have on my treatment needs/quality of life preferences now, only for his life after me to be significantly worse off, financially? It’s his life, his money, too.
Ok, so costs are up, some through choice and some through imposition by others. Then there is the whole matter of income. Would working be feasible while getting treatment and was I entitled to any income support? I’d just applied for two great part-time roles to go with the independent projects I was working on. I put the applications on hold. The weekly schedule of hospital appointments, blood tests and Chemo didn’t seem to leave room for work. Working as I had planned to work, seemed impossible. Not knowing how I would cope with Chemo and how much rest I would need also made it difficult to commit to a new job. I didn’t want to let others down and I would need flexibility. I’m not sure I would have hired me in those circumstances.
Costs have gone up and kicker number two; earnings have come down, crashing down. I know some people work while receiving treatment, through preference for the distraction or normality of working. Some people work because they must. Others can’t work through being too ill and rely on income support through disability or illness. The overall equation is simple; less income in, new costs and normal costs doubling, mean less money overall, fewer choices and for most people, more stress and pressure, right at a time when resilience, calm and mental strength are needed.
How do people living with cancer cope? How can I cope? Even the idea that I would need to consider income support played with my sense of self, sense of standing on my own two feet, being independent, contributing and not being a burden. Yes, I know, I can hear some advice now, the support is there for these kind of times, when unforeseen circumstances hit, you’ve paid your taxes for twenty years, you’re entitled to support, take it. It still irks and I’m working through what I can and can’t claim, how much I can and can’t work, whether work is helpful or unhelpful, an option financially or not.
There has been a wee light at the beginning of this cancer cost journey; the small critical illness insurance I did have, was paid out within 10 days without quibble. I am forever grateful for this, for one insurance company’s sensitive, rapid handling of my claim. They made sure they didn’t add any more stress to a very stressful period of wrapping my head around diagnosis, the very opposite response of the travel insurer.
The challenge now is to turn this wee bit of money into considerably more money and find the time, amongst all the treatment, for this whole other project – changing our finances for our new circumstances. I feel so awful for my husband in all of this; he didn’t sign up for his quality of life to be diminished, his wife to be ill and more pressure on him to earn and yet simultaneously be with me at treatments and consultations. We certainly hadn’t included hospitals and medications and thoughts about selling our home, in the design of our near future. Yet, I know in so many ways we are lucky and many people don’t have choices financially or otherwise, in the way that I do, we do. Though sometimes I don’t feel very lucky.
Cancer costs; not just emotionally, physically, spiritually, intimately – it costs financially, in all sorts of directions, I couldn’t have anticipated and know that I am yet to encounter. I’m not yet facing that scary prospect of needing an experimental drug not yet available in the UK or a trip to the USA for a new type of Car-T cell treatment or new transplant. Those do not bear thinking about right now.
Talking about money is hard; it is so often a contentious topic or a trigger for stress. People often have very different views about money and very different relationships with money. It can be hard to find agreement with the ones we love about how money should be earned, spent, saved and valued and that is when life is going well. When illness strikes or circumstances change, it becomes even more important to set aside any fear, vulnerability and embarrassment arising when talking about money. I recommend taking a deep breath and just start talking about it, in a matter of fact manner; your financial mistakes, lessons learned, fears and hopes. One hope I have is that this post helps others talk and listen to conversation about money in a compassionate and non-judgemental way. In cancer journeys, along with other life journeys, agreeing how to move forward financially is important and warrants open honesty. This will help money worries and any negative impact on recovery and treatment outcomes for the person living with cancer and their loved ones to be minimised.
1Chemo’d (my new word, do you like it? Or I could just say ‘fried’ but I like Chemo’d better, more self-explanatory I hope)
Acknowledgements:
Editing: Isobel S
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Finance and Cost, Psychology for Cancer Tagged with: Cancer, Hidden Costs, honest, Money, Myeloma, open, Talk, Treatment
June 13th, 2017 by Janine

I have learned a lot about generosity over the last few months. Generosity is something I now realise I have made difficult for others at times and I have not always felt comfortable, when in receipt of it. Generosity can be a strange thing. It can feel like receiving a compliment: pleasant, appreciated yet also sometimes awkward. Awkwardness can depend on how often or intensely delivered the compliment is, and how much I believe it is well intentioned, genuine or even believable. Most often, generosity, offers for help, people taking the initiative to think about someone’s needs and meet them without asking, is very much appreciated and immensely supportive and loving.
Other times though, over-generosity is experienced. This is generosity where what I might be saying about my desire or needs isn’t heard, or is heard but ignored in some way. It can feel disrespectful and invalidating, and take away my independence. I can then be left with conflicted feelings of guilt for not being appreciative enough and annoyance at not being listened to, or believed, about knowing my own needs better than another. It occurs to me that older adults or people living with learning or physical disabilities may feel like this on a frequent basis. This feeling hasn’t often happened to me yet, though has occurred often enough to finally make me stop and think, about how I might impact others when trying to give or be generous. It has especially made me think about my relationship with my parents and extended family regarding giving. It hasn’t always been easy to work out how to give in a way that meets everyone’s preferences or budgets (so people are not left feeling embarrassed or like they need to match the budget when being generous themselves) and still leave a lovely sense of giving, and an appropriate sense of pleasure and gratitude in the receiver.
My logic about it making sense for me to pay for something, during times when I have earnt more or been on a favourable exchange rate or simply wish to be generous as a way of showing love (like feeding people), doesn’t always fit with others desires to pay their own way, use the monies they have put aside for exactly this type of expenditure and retain control over the product, service, experience and spending for themselves. Ironically too, these are preferences I also value and wish to exert when someone is being overly generous with me. Of course, talking about it honestly is a good remedy and preventative measure; one that will be put to the test in upcoming months as Mum and Dad visit. The last thing I wish them to feel is undermined or disrespected in any way.
Generosity is not all about money or gifts, it can also become too much when it involves doing things for others. Doing things that another person doesn’t want or need, or doing something that only partly fits a person needs, can be difficult to receive. The receiver can find themselves having to manage the other person’s feelings; how to be grateful and appreciative while considering whether anything is said about ‘please don’t do that again’ or ‘that’s so generous and unfortunately I can’t use/eat/keep it’. Instead of feeling helped and supported, the very person the giver wished to support, can be left feeling with ‘another thing to do’, ‘anxious’ or ‘overwhelmed’ and at worse wanting to withdraw from and push away a person or others’ offers of help.
Generosity’s foibles
Studies show that there appear to be many motivational, cognitive, and situational factors that influence helping behaviour and altruism1. Giving and receiving is not as simple as we might think; arousal and emotions are involved. Both givers and receivers don’t always get what they hope for.
Whereas giving a gift out of guilt is linked to the giver feeling more of a connected relationship, receiving a gift, given out of gratitude, is linked to feeling a more connected relationship. Giver and receiver experiences can be very lopsided in each generosity interaction.2
Similarly, to selfishness, too much selflessness may lead to rejection. It can be viewed by receiving others as undesirable, causing discomfort by highlighting gaps in their own virtues or be deemed to be socially rule breaking.3
Summary
Generosity is a curious beast, worthy of reflection and application of open communication to ensure it doesn’t slip over from loving support to being unhelpful and disrespectful. Hopefully my understanding evolves over time and becomes easier, more balanced and my levels of giving become appropriate and intuitive.
Acknowledgements
1 Dovidio, J. F. (1984). Helping behavior and altruism: An empirical and conceptual overview. Advances in experimental social psychology, 17, 361-427.
http://www.sciencedirect.com/science/article/pii/
2 Chan, C., Mogilner, C., & Van Boven, L. (2014). Gratitude, Guilt, and Gift Giving. NA-Advances in Consumer Research Volume 42.
http://acrwebsite.org/volumes/1017574/volumes/v42/NA-42
3 Parks, C. D., & Stone, A. B. (2010). The desire to expel unselfish members from the group. Journal of personality and social psychology, 99(2), 303.
https://www.ncbi.nlm.nih.gov/pubmed/20658845
Editorial Support: Stephanie Kemp
Illustration: Sapphire Weerakone
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Psychology for Cancer Tagged with: arousal, Cancer, emotions, Generosity, Myeloma, Psychology, Receiving Help, Reflection
I bopped down the hospital corridor towards the Chemo Unit (listening to a bit of Adele) and started thinking back over this cycle of treatment. It’s not a good or bad news story. It’s a GREAT news story. Yes, there are a few side lines about niggly things, just to keep it real. Great news though; we can always do with a bit of that, can’t we?
Music – Music was back, yay! All a bit eclectic, and hey, that’s how I roll!
The theme-tune from Cheers: Where Everybody Knows Your Name, Gary Portnoy; On the Level, Mac DeMarco (calming and grating at same time); The Only Way Is Up, Yazz; Rapture, Blondie; An hour of Radio 1 in an afternoon; Right as Rain, Adele (transpose talk of lover with Myeloma; it works!)
Also gobbled up podcast S-Town, Serial Series 2 (Series 1 was great too).

Medical Update
Here’s a graph. I love a good graph, don’t you? I especially love this one as it shows some important stuff going in a mighty good direction. Cancer presence is trending down. My chemo response rate is trending up! Yeah, baby!!! I’m not fighting with Myeloma; I am guiding it to the door, hoping ultimately to close the door behind it for as long as possible.
The great news
My para-protein level, the indicator of those unwanted Myeloma plasma cells (now kicked to dust over the first two cycles of Chemo) is looking good, very good. My results have come down: from 40 g/l at diagnosis, up at 42 g/l when starting treatment, down to 17g/l by the early part of this cycle and by the third week, 11 g/l. The medical team look for (and the clinical trial requires for next step progression) a minimum of partial response (PR) by the end of the induction treatment (four cycles of Chemo). PR is a drop of 50% of presence of Myeloma indicated initially by the para protein level. The good news is that I had achieved PR by the end of Cycle Two! Also, the para protein level has kept heading in the right direction: down! I still have one cycle to go in this round so a great overall response rate seems so possible right now. And I am still gunning for 100%. I hope I am not too disappointed if 100% is not achieved.
The niggly things

It was a tough start to Cycle Three. I was feeling a bit low. On day one, Si and I attended a clinic appointment with my Clinical Trial lead. It was helpful, and he kicked off the conversation about the stem cell harvest. It was also awful. He went over the prognosis again: the incurable nature of Myeloma. Then he followed with the dramatic strides that have been made in the last two years with new drugs and better outcomes. They are better outcomes: people with Myeloma receiving treatment used to get three years, recently they were getting seven, and now the average is 8-10 years. Great strides, but still short, and I had trouble on that day hearing it all again. I wanted to focus on next steps in the treatment instead, not how long it may or may not ‘get’ me. I left feeling utterly drained and not overly well-informed about the cell collection as I had trouble listening to these points with loads of the other stuff in my mind creating noise.

While the scaredy needles seemed to get over their fear this month (Nurse L worked her magic), a strange rash appeared down my left arm (worse than the little bit I had experienced in early days of Chemo) and it hung about for a couple of days. No known cause at this stage and something to look out for again. My calcium level dropped a bit so I now take calcium tablets too. My urea and creatinine levels dropped for a week. These returned to normal after I focussed on keeping up the three litres of water a day and recognised night sweats might be dehydrating me a bit more than I had thought.
Long waits for Chemo occurred on a few days. One day was over three hours and down to a process issue; these kind of things happen sometimes yet are usually preventable. I gave what I hope was constructive and gentle feedback to the medical team. They were supportive, listened really well and agreed a plan of action. A Clinical Trial Nurse, M, thanked me for being an active partner in my treatment: for my feedback and follow up on things they have mentioned in the past, such as providing patient diaries and requesting new ones if they have not been received. Her comment felt genuine and I really appreciated it. I never want to overstep or cause additional work, yet my nose for process re-engineering and efficiency often rears its head, especially in the NHS. The NHS is awesome (free!) and could benefit from regular process review, especially as when used well, reviews and service/process development ultimately save time and cost. Hey, who has time to do timely reviews? More appropriate NHS resources required! Let’s hope Brexit doesn’t scupper that. Or the upcoming election.
Other great things; small and large
I attended a helpful webinar through MMRF that shared the latest USA understanding and treatments. Lots of promising diagnosis tools and new drugs are coming down the line that will hopefully be available in the UK by the time I need them, after my initial remission period lapses. I also attended a fabulous day at Kings College Hospital where the latest UK-based clinical trial information and outcomes were shared. We were given a tour of the labs in which blood and marrow are analysed, stored (at -196 degrees) and the clinical research facility. After donning the blue plastic shoes, hair bands and protectors to ensure we didn’t cause any contamination, we were taken into one part of the facility where we could safely view the highly-restricted areas and complex equipment – very ‘CSI’ (for anyone who has watched those TV programmes as much as I have). We learned about how contamination is monitored and prevented, and how studies of highly sensitive blood and organs are undertaken. Fascinating, and a real privilege to see ‘behind the scenes’ in this way.
My girlfriend B came along to Chemo with me on day 2 this month and it was so great to have her there. She was calm in a strange environment and we laughed together which was fab. Strangely, despite the circumstances, this day and another day on which we did meditation together and a third day when we made time for a great lunch date (unfortunately just before she left London; would have been great to fit in more of these) really stood out to me as special moments, quality time and very supportive.

We finally christened the table tennis table (Si’s birthday present). I am queen of the table; the presiding champion in the round robin between Si, my brother-in-law and me. Of course, were you ever in any doubt? Si didn’t like that and brought up other stories about me beating him at clay-pigeon shooting over ten years ago during another birthday present experience for him. Ooops! Although, wait until Mum gets here, she tends to claim table tennis crowns!

On the last day of Chemo this month, I wore a dress and two people told me I looked lovely. What a great start to the day. Especially as I felt very tired that morning. Choices again. I could have worn tracky bottoms and a top like I did the day before and that would have been fine. I needed a pick-me-up. A dress and makeup was a helpful move. After all, I felt better. It was great to dance in on the way up to Hospital, feeling the fabric move around my bod. And hey, it resulted in compliments – the dress, not the dancing! Worth it, that little bit of effort. I might not have the energy to do this next time and that’s ok. It was lovely to grab the moment on that day.
Thank you
Thank you to you, the readers; there are now over 800 users on the Psyching Out Cancer blog.
Psychology – Reflection
Life is a daily, weekly, yearly roller-coaster of good, difficult and neutral events that come and go. Our response to each event – small or huge, the attention we give each, the meaning we add, the willingness to accept the unchangeable – all dictate how we well we cope with the rollercoaster. Our ability to pause, notice, and choose a response, facilitates how much we stop and enjoy the good times, and ensures the more difficult times have less impact on our day to day lives and long term goals. Sometimes though, we forget to pause or find it difficult to pause; this is where in addition to knowing our triggers for unpleasant reactions, Reflection is crucial.
Reflection is defined as serious thought or consideration. In psychology, reflection often involves a therapist reading or saying the client’s words back to the client so that they can hear for themselves what they have said and evaluate the logic or reasoning behind their own statements. You can also be your own therapist with reflection. Self-reflection can be referred to as examination and contemplation of our own thoughts and behaviour; helping ourselves to hear and evaluate.1-3
There can be no knowledge without emotion. We may be aware of a truth, yet until we have felt its force, it is not ours. To the cognition of the brain must be added the experience of the soul.
Arnold Bennett (1867–1931) 4
The lessons I have learned, and psychology skills I have applied, this month have often been difficult to remember to use in a timely manner and I have needed time to notice and understand my reaction and needs. The post reflection lessons have been transformative and confronting; they have led to open, honest debate with myself and communication with others such as in my previous post ‘Killing Me with Kindness’.
All in the Mind, a BBC Radio show presented by Claudia Hammond, is a fabulous resource for learning about mental health (links below). The show often hears from people with experience of mental health difficulties, charities working in this space, expert clinicians, and academics and researchers who explain the latest evidence about incidence and treatment, and debunk myths. In one of the recent episodes, evidence was presented about the power of expressive writing about your experiences and the positive outcomes that were experienced.
Writing can be, for some, a great way to facilitate reflection. Whether it is keeping a diary, or writing a letter to yourself or another, writing about how events made you feel emotionally and physically, the thoughts you noticed, what you were curious about or wondered about in terms of the event, yourself, the other person’s thinking, feelings, reaction, motivations. It can be so helpful to ‘not to make the person wrong’. Instead, focus on the event or behaviour and how it made you feel, how you thought it might have made the other person feel, with curiosity and compassion. Recognise that you may have their feelings and thoughts wrong; be careful not to assume and instead be curious. You do NOT have to send the letter. You do NOT have to keep the letter once it is written, though you may find it helpful to send or re-read them; only you can decide this.
For those that don’t like writing, a Dictaphone, a voice recorder, or even an app that converts your voice to word or pages can be used.
If neither of these appeals, taking time out simply to be and think about a past event, day, week, a particular period, can be useful. Notice all those things above, and also notice what worked well, what worked less well, and what you would do differently or not do differently.
Alternatively, and I highly recommend this approach (which can be done alone or in combination with the others above) solely focus on taking time to sit, put yourself back into the event and be with whichever emotions, light or strong, arise. Allow yourself to feel them, deeply, outwardly with tears, or anger or another response, if that is what arises, without judgement of yourself or anyone else. This type of reflection helps your body and mind to fully experience and process events together. Regular reflection, not rumination where negative thoughts are given repeated attention, but regular curiosity-based reflection, can help process strong emotions.
All regular reflection can help your mind and body notice when similar events are happening again, often earlier than usual, and sometimes even in the moment. This observation then allows for pause and choice of response; helpful or unhelpful, one that serves you well or doesn’t serve you well.
Remember, after reflection, be kind to yourself; your responses and emotions within reflection are normal. If you feel upset or angry afterwards, take 5 minutes or more to do something enjoyable even for a few minutes; take a few deep slow breaths; tell yourself you are ok, safe, good enough; read a magazine; do one yoga sun salutation; make a cup of coffee; close your eyes; do a body relaxation exercise, a tai chi movement, a back stretch or something else relaxing and fun to bring your arousal level down before trying to get on with your day.
Summary
Reflection is an important skill for maintaining good mental health and one worth investing time in practicing: through writing, dictating or focussing on your experience in a curious way that allows you to fully experience your emotions.
Great News
Cycle Three – done. A roller-coaster and many highlights of great news. Onwards with Cycle Four, the last month of Chemo before the next phase of treatment. Gosh, the time has gone quickly.
Resources
BBC – All in the Mind. http://www.bbc.co.uk/programmes/b006qxx9
All In The Mind, Episode including benefits of expressive writing (15 May 17) http://www.bbc.co.uk/programmes/b08n2wcz
Gibbs Reflective Cycle (in Dye, 2011), University of Cumbria (2016)
http://my.cumbria.ac.uk/Public/LISS/Documents/skillsatcumbria/ReflectiveCycleGibbs.pdf
Acknowledgements
1 Oxford Dictionaries https://en.oxforddictionaries.com/definition/reflection
2 Alley Dog Psychology Glossary https://www.alleydog.com/glossary/definition.php?term=Reflection
3 Psychology Dictionary http://psychologydictionary.org/self-reflection/
4 A return to the use of emotion and reflection. Helen Demetriou and Elaine Wilson
https://thepsychologist.bps.org.uk/volume-21/edition-11/return-use-emotion-and-reflection
Images: B, Me
Editorial Support: Stephanie Kemp
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Chemotherapy for Myeloma, Myeloma Treatment Tagged with: Cancer, Myeloma, Para Protein, Partial Response, Psychology, Reflection, Response Rate, Survival Rates
I am vegetable. Literally. I am consuming so many of them and have lost weight (under 65kg) either through this crazy new diet and/ or the Chemo, that what is left of me has re-constituted itself. I swear it! Green goes in and green comes out (sorry). I collect sunshine where I can. I am drinking all the water I can get. With this combo, I reckon I’m probably embracing photosynthesis, absorbing energy through chlorophyll and soon I will be producing oxygen, instead of consuming it. Really, I am now a green vegetable!

Last week, I talked about the decision to change my terrain. Nutrition was my first target area. There are a multitude of varied opinions about Nutrition for Cancer out there in the world. Some are downright scary. Advice to avoid medical treatment and ‘cure’ yourself by changing nutrition, is frankly, dangerous for many individuals and their individual cancer journey. Other advice, such as all fruit is great, can also be spurious; grapefruit is known to mess with chemotherapy.
The people you might think would know about this field, be trained in this field, are not! When first diagnosed, I asked my specialist Myeloma team, “What can I do to help?”, “What should I eat?” I was keen to explore how could I change my diet so that my body;
- doesn’t remain a cancer heaven where Myeloma thrives,
- could tolerate Chemo well, and,
- becomes an environment that facilitates optimum Chemo effectiveness.
Their answer shocked me, sort of. “They didn’t know” and explained, “We don’t receive training in Nutrition”. This was disappointing. I needed advice.
Partners in Nutrition
I felt sad and a bit frustrated that my clinical team couldn’t offer anything comprehensive on the topic. On the upside, I knew they were doing the best they could in their speciality area, and were focussed! After my questions, they asked ME what I was doing, which vitamins I was taking and what I was thinking of changing. ‘Thorough of them, to ask’, I thought. However, the discussion felt the wrong way around and left me hanging out there, without the very partners, I thought I would have, on this ‘changing my terrain’ journey. I realised I would have to look elsewhere.
I wanted to be as informed as I could be in Nutrition for Cancer/Myeloma, without inviting so many alternative approaches, that the options became difficult to manage, or difficult to make decisions about. I decided to seek advice from three specialists: the hospital dietician, a Haematologist in the wider medical team who Macmillan recommended, and a private Nutrition Therapist, recommended by a neighbour. This person had trained in Nutrition after her husband was diagnosed with cancer and she had experienced her own health challenges. These three key consultations, the anti-cancer book I have mentioned previously and, two friends with their wealth of nutrition knowledge and experience, seemed more than enough sources of information to start with.
Consultation and Decision
I felt in control (Ha! That word again!) and purposeful. Yes, this whole nutrition thing was yet another project within the whole managing cancer project; it was ‘full on’ but it also felt good. I was doing something to help myself, rather than everything happening to me.
The consultations were very different and all very helpful. While there were some mixed messages, often I was able to double check key points learned from one with another and hear another rationale about why something should be left on or off the menu. Ultimately, I very much appreciated everyone’s efforts and time, especially where it was given for free and I felt informed enough to make my own choice.
The Hospital Dietician (free 30 minute call): Helpful, friendly, most concerned about my weight going in the right direction; not going into free fall. Recommended more of the standard balanced diet we generally hear about in the media, eating without denial and to feel good, and, cake was probably a good thing for getting the calories in. Didn’t seem to have any specific cancer related advice though it may be that I felt fairly informed by the time I spoke with her.
The Haematologist with a personal interest in Nutrition for Cancer (free 60 min call): Very helpful and passionate, advocated a ‘Plant food’ and ‘some dairy’ only approach. Coffee, if needed, should be good quality and better to avoid decaf coffee altogether as it is often processed with chemicals. No sugar though sugar substitutes are OK (e.g. agave, stevia) but not artificial sweeteners. Recommended several interesting books (included in the links page on this blog).
The Private Nutrition Therapist, C, known for her work with people living with cancer and undergoing Chemo (paid for 60-minute face to face, plus two 30-minute skype follow ups): Easy and professional to work with, also passionate and overall, clear about her recommendations and rationale. Adapted her style knowing I like the science and evidence, which I greatly appreciated. Advocated a full comprehensive plan of dietary and lifestyle changes tailored to my specific needs.
I went with the last option as my base approach. I had found my partner in nutrition for Janine’s Myeloma. A relief washed over me. Phew. I wasn’t going to have to work this out alone.
Now, I am a vegetable.
New way of eating
The new eating plan aimed to support my body through the induction treatment, the initial four to five-months of Chemo. Things may become more flexible later (I hope so!) to support specific medical procedures like a stem cell transplant, remission or a maintenance phase. For now, a complete revamp was proposed.
Important
Please note that I have not provided the nutritionist therapist’s full plan in detail or my own adaptations to it, in full detail, as my regime is specific to me and my circumstances. It may not be appropriate for everyone.
For the last three months, I have stuck as closely as possible to:
- No Gluten
- No Diary
- No Sugar (including natural sugar).
- No Alcohol
- No Coffee
- No Processed Food
- No Low Quality Salt or Table Salt
- No Soya (unless tofu)
- Eat (A LOT OF) Organic vegetables or vegetables from known low pesticide/nasties source
- Eat Organic, Wild, Grass-fed (as applicable for product) meat, fish and poultry only.
- Take Recommended Supplements – to provide nature’s natural chemotherapy, enhance the immune system, reduce inflammation, support the nervous system, prevent mouth ulcers (common during chemo) and latterly, regulate body functions and build body mass.
- Avoid other supplements – can interfere with Chemo
Plus, the medical team directive:
- Drink three litres of water daily – I am a water-logged vegetable. Glug.
- Take daily and weekly Meds
- Infuse weekly Chemo.
- Avoid grapefruit – interferes with Chemo (an example of nutrition studies that have been done and with a helpful outcome).
Yummy-less.
Let’s pause and think about that for a moment. I love food. Food is always a big part of any travelling I do and I take a LOT of pleasure from food. This was going to be painful – no gorgeous oozy mozzarella (dairy), no Ham; prosciutto or Parma (processed), no fresh ravioli (usually with ricotta so dairy and gluten), no Greek yoghurt (dairy) which I adore. For the Kiwi British comfort eater – also painful – no toast and butter (gluten and dairy and sugar; in the bread!), no bacon (processed; I so miss this!), no cheese melts, no crisps (processed and often with sugar and less than ideal oils – corn syrup, vegetable oil, rapeseed oil), no fish and chips (‘bad’ oil, gluten), no pies (I’d just found a great provider in Borough market and started getting them as the odd treat, not anymore), no cake (aaargh!), no dark chocolate hobnobs (gluten, sugar, dairy), no chocolate (!!!), no flat whites, no cappuccino, (no coffee for me, the coffee addict), no standard milk, no champagne, no margaritas, no red wine. No, no, no, to all the yummy things and the vast list of other foods that help make things yummy. No grabbing a sandwich from a café when on the run (majority are processed, have poor quality salt and a ton of added sugar – look out for anything ending in ‘ose’ like dextrose (it’s all sugar). Not only is anything yummy seemingly out, now my whole relationship with food will need to change; I will have to be super prepared before leaving the house and in-house! Sounds like a Mum with kids to feed but I’m not a Mum and one of the benefits of that, up until now, is that I had been able to be more spontaneous over food.

‘Figuring out’ and the challenges
I couldn’t do it. This was going to be too hard. There wasn’t going to be anything left to eat! Especially with the no natural sugar thing. I checked in again with C about whether I really did have to give up natural sugar. I was reminded that Cancer seems to LOVE and I mean LOOOOOOVVVE sugar. We agreed that if I have too have fruit (and I do) I would make it no more than 1-2 pieces a day and ideally only ‘good fruit’ – high in antioxidants and/or low in natural sugars.
Working out what I can eat and trying it out over the last three months has been very, very, time consuming. I wanted to embrace the new plan and do the best that I could do but I did wonder if I would be determined and disciplined enough. Funny how focussed you can get when pain, disability and death loom large.
I felt fortunate that some recommendations landed more lightly and didn’t have the combined bulldozer-tornado effect of others. Over the last ten years, I had considerably reduced my bread consumption to avoid gluten (I had felt bloated and low energy after eating it) though this had been harder to resist lately, with the abundance of gorgeous sourdough loaves on every corner. I haven’t drunk a lot of alcohol either. My average intake has been less than one unit per week for years so this restriction was also easy; only hard when out with friends and celebrating. I had recently cut down my coffee consumption to a maximum of two a day (my Uni colleagues may not believe this!) and I have used lactose free milk with coffee for several years.
I hoped these pre-diagnosis adaptations meant I was off to a good start. I knew getting vegetables in when I don’t overly like many vegetables and often find the ones available in the UK tasteless, was going to be a major hurdle. Unbeknown to me in the early weeks of this new regime, this hurdle was not the greatest nutrition challenge I would face.
Consuming enough calories and slowing my weight loss (never thought I’d say that) has proved to be very difficult. Finding my groove with food, and food routines, and figuring it all out so that it doesn’t take up most of the day, has been a huge journey; one that continues. Eating out and stopping myself from getting excited when seeing something is gluten and dairy free as it is often still full of sugar and off limits has been tough. Seeing blocks of cheese left in my fridge by others, really wanting a piece, that’s been hard too. Even my hubby doesn’t eat cheese so we’d both rather it wasn’t there (now binned but felt wasteful). Finding solutions that work without becoming evangelical about it, or a boring, pain in the arse…well, that’s been hard too.
What DO I eat and do I LIKE it?
Standing at the kitchen bench each morning in the early days; I felt like I needed to do a warm up to get ready for the next three hours ahead, the way you might before heading out to bootcamp, the gym or for a run. Have you ever tried to make sure you get enough food and fluid in, early in the day, so that you;
- can take all your meds on a full stomach,
- get enough calories in for the day, and
- consume enough, early enough so that you do not have to get up every two minutes during the night for the loo, and manage to get some sleep?!!
It takes something. I often feel baby-esq, permanently attached to a water bottle, only putting the bottle down to eat something that usually involves a nut, vegetable, powder or all of them at once.
Can you picture the cliché movie scene where the main actor is using a blender and the stuff that is meant to be blended (usually a lovely red or green colour) ends up all over the actor, walls, and floors? Well, welcome to my world. I have had a few of those moments, and cried. Rushing around when using a Nutri-bullet or Vitamix blender, isn’t recommended. Paying attention is. Trying to do the right thing, get in all the nutrition self-care, and prepping stuff to take with me, before heading off for a day of treatment is hard work. I can feel exhausted before I’ve started. Now after my initial stuff ups and clean ups, my Nutri-bullet is a friend. I thank the Universe for its prowess in whizzing up material in to a consumable form that I otherwise would have avoided like the plague.
I down a bottle of warm water with apple cider vinegar first thing and then get on with washing green veggies (spinach, cavalo nero, kale, cucumber…) acquired at the Sunday morning market. I stuff them in to the Nutri-bullet container, add in a tablespoon of sprouted broccoli powder (elusive stuff, frequently out of stock and gratefully received as if it were gold ingots from my girlfriend who recently hauled it all the way from NZ), add turmeric with black pepper (great anti-inflam), lemon juice, water, coconut water or almond milk, a piece of apple or a plum or ten blueberries and whizz!
I down it quickly, it’s not unpleasant, sometimes it’s even nice, I just find it easier this way. I get full quickly and I risk not getting the whole thing in, if I put it down and say to myself, I’ll come back to it, I do but by then it’s 11pm and I’m trying to finish off the water I’ve also missed and get to bed. I leave an inch of the green stuff in the bottom of the container for round two; the hard-core elements. To this I add psyllium powder, rice protein (like cardboard) or another protein powder (a new addition to try and up the good calories), flaxseeds and any other good for you gook that congeals quickly – whizz well and drink instantly. A tiny bit of pineapple juice can help, if it really tastes naff. Then I usually race up the hill to have a blood test. With a water bottle.
Next I work on my second breakfast. If I don’t try for four meals a day plus snacks I don’t get anywhere near 1800-2000 calories a day and I just keep losing weight. Crazy! Eggs usually, or porridge with nuts or oily fish…essentially some type protein and maybe a few more veg. I seem to live on avocados and rice cakes with sardines in olive oil these days. Lately I have had success making gluten free bread and nut bread so poached and fried eggs (in coconut or avocado oil) have returned with a vengeance and I love them. Slowly I am managing to find or make alternatives to most of the yumminess products I listed above that are either similar enough in taste or texture so that I don’t feel I am missing out. I make my own turmeric and cacao lattes with almond milk, my own nut butter, my own dairy and sugar free mayo. If I fancy something like bacon, I try to figure out what might be closest, like organic ham hock and have a go at cooking that. It was close enough to abate my hankering for a while and I didn’t feel like I was denying myself something I love.
I had sausages this morning – god they were good. It’s very hard to find good quality, gluten, sugar and dairy free sausages that use organic, free ranged meat unless you order a minimum of 5 kilos from a great butcher. I found some today and along with the organic mushrooms and eggs, I was in heaven. See, its not all bad.
Lunches and dinners are not that different from before all of this; they just include more of a psychedelic rainbow of vegetables with the protein. Roast chicken (organic) still on the menu. Yee ha!
The power of ginger
Three ginger tea is also godsend (or Universe-send). It has been my personal miracle tonic. When I have felt nauseous from Chemo instead of reaching for the Dom (domperidol), usually, a cup of ginger tea has stopped the nausea in its tracks. I am very grateful for this. I already take enough meds so didn’t want to be taking Dom all of the time too (it’s a three times per day, kind of drug) and one I am probably going to need later, when the going gets even tougher.
Eating Out
I love café and restaurant culture. I don’t go out quite so often anymore, so that I can control what goes in to my body but when I do I tend to choose vegan cafés or those that have egg or gluten free options where possible. Thank goodness London has transformed in this arena over the last five to ten years; it is much easier to find ‘free from’ options now or menus that have gluten free alternatives.
However, it is much much harder to find menus and cafes that have options that are gluten, dairy AND sugar free or that don’t then include a vegetable or rapeseed oil or some nasty unnecessary non-natural additive. Some places like Whole Foods, Deliciously Ella and independent farmers market stall holders are good and expanding their ranges all the time. Although, after going to these places once or twice or when their menu doesn’t change, it can be hard to find as much pleasure in eating out. The ‘healthy’ places are not prolific like the other major café houses so finding them when you need them can be a mission too or require a special trip.
It is also frustrating when going into a place that has set itself up with a healthy eating concept only to discover the alternative milk they have on offer for making flat whites or lattes are brands that include a whole lot of unnecessary sh*t in their product such as unnatural flavouring and sugar. This makes me especially mad when there are other available brands which are simply almonds and water or almonds, water and Himalayan salt or simply coconut milk alone. Yes, me and my gobby (frustrated) mouth. I do usually point this out and ask them to consider other brands. In all fairness most places, especially the smaller independent ones have showed interest in doing just that.
Upsides
There have been some fantastic upsides to sticking with this plan and coping with its strictness.
- Food tastes better! Even vegetables! They often taste sweet! I taste the natural sugar in everything and still enjoy savoury flavours too.
- I feel better. I do. Setting aside some of the related and intermittent presence of Chemo side effects (low appetite, metallic taste in my mouth, fatigue), I feel better than I have in years. It may be psychosomatic but who cares?! I feel cleaner on the inside. I look better on the outside. My whole digestion system seems to be working better and this is after years and years of struggling with irritable bowel symptoms! My skin is clear, soft and the keratosis has improved dramatically.
- My stomach is flatter, I rarely feel bloated and I’m quickly able to tell if my body likes a food or not because it reacts so quickly when it doesn’t like it; I presume because the rest of the environment is becoming optimised.
- I have lost the weight from those places I have always wanted to lose weight from. While Chemo may have contributed to overall weight loss I do think the new way of eating has contributing more to my vamoosing the fat. I have reached this conclusion because many people find they put on weight with the steroids included in Chemo and in the past when I have had to take steroids, I have put on over two stone quickly. Instead, this time when taking a reasonably high dose of steroids, I have lost weight. I think my new diet has been the biggest contributor to my fat loss and Chemo may have contributed more to loss of muscle mass. Therefore, if a person not undergoing Chemo, tried this way of eating, particularly the major reduction in sugar, increasing the plant food, and removing processed foods, I suspect they would lose weight without losing lean muscle.
- I’ve learnt to make healthy products that I had always wanted to learn how to make. Nearly a decade ago, just before the tide turned in London and it began to welcome free-from and health-food, I had started investigating developing a gluten-free product line but didn’t get it off the ground. I’ve watched as my ideas were executed brilliantly by others and took heart that I had been on the right track.
- Another upside is the abandoned, unloved bread making machine has risen from the dead and is now a cherished kitchen tool, used regularly.
The other and most important major benefit that I am choosing to ‘step into’ is that this new way of eating has majorly contributed to how well my body has tolerated Chemo so far and how effective the Chemo has been; helping me to significantly reduce the unwanted para-protein level in my blood after only two of the initial four cycles of Chemotherapy. My clinicians are pleased. I am pleased.
Lapses
It doesn’t mean I have been a saint and stuck totally faithfully to the plan. I am only human and we have been born and bred on sugar so lets face it, I was never going to kick it completely and easily. Overall, I have been feeling rather virtuous about my avoidance of the stuff and any other nasties but there have been lapses.
In an earlier post, I confessed to an indulgence of coffee and cake on Si’s birthday. I also confessed to savouring a coffee on another day – more about coffee below. The biggest lapse came like a smack in the face and I learnt my lesson. For two days, I fell off the wagon and in particular, allowed dairy, to creep in. Boy, did I pay the price. At both ends. A different shade of green, I ended up in bed for a day and weak for five. My skin went to pack. To recover, my body craved green smoothies and strict eating. It really was a wakeup call about how much better my body had been feeling overall, beforehand, despite the Chemo effects. Dairy has been out, out, out ever since.
Strict versus living
I have recently adjusted my plan to allow for one, occasionally two coffees (weekends) with almond milk per day. I love coffee so much, the smell, the ritual, the taste. As it does have some health benefits, I decided life was too short (ha!) to go without this love. Most importantly, I have learnt to drink it when I stop, pause, and rest, instead of using it to replace food, as a stress release or to ‘keep going’.
Picture my local organic health food shop. It’s a throwback to the heady hippy days of the 70s, where weird looking products on home-made wooden shelves, are caressed by music from a display of vinyl records, lovingly played on an ancient turntable at the back of the shop. This place provides the most divine items, for those times, when I just can’t go without sweet treats, any longer. An amazing gluten free, dairy free, smooth, creamy (from avocado not cream) dark chocolate tart is the star. The trade-off is that alongside the high purity chocolate, it does have some agave in it (a natural sugar substitute). I have had this twice now and thoroughly loved it. I plan to make it myself so I can control the sweet element even further, and use the tiniest amount of rice syrup rather than agave.
Is it worth it?
Well so far, my new eating plan has been in existence for the same amount of time that my test results have been improving. Maybe, just maybe, eating this way, going without some foods I love and embracing new foods and new ways of consuming them, will extend my life. Just maybe, it will extend the quality of my life. At the very least, just maybe, it will enable me to cope well with treatment and avoid common complications; kidney and liver failure.
I am a skinny green vegetable.
Cancer. Don’t eat me.
Acknowledgements:
Illustrations: Sapphire Weerakone.
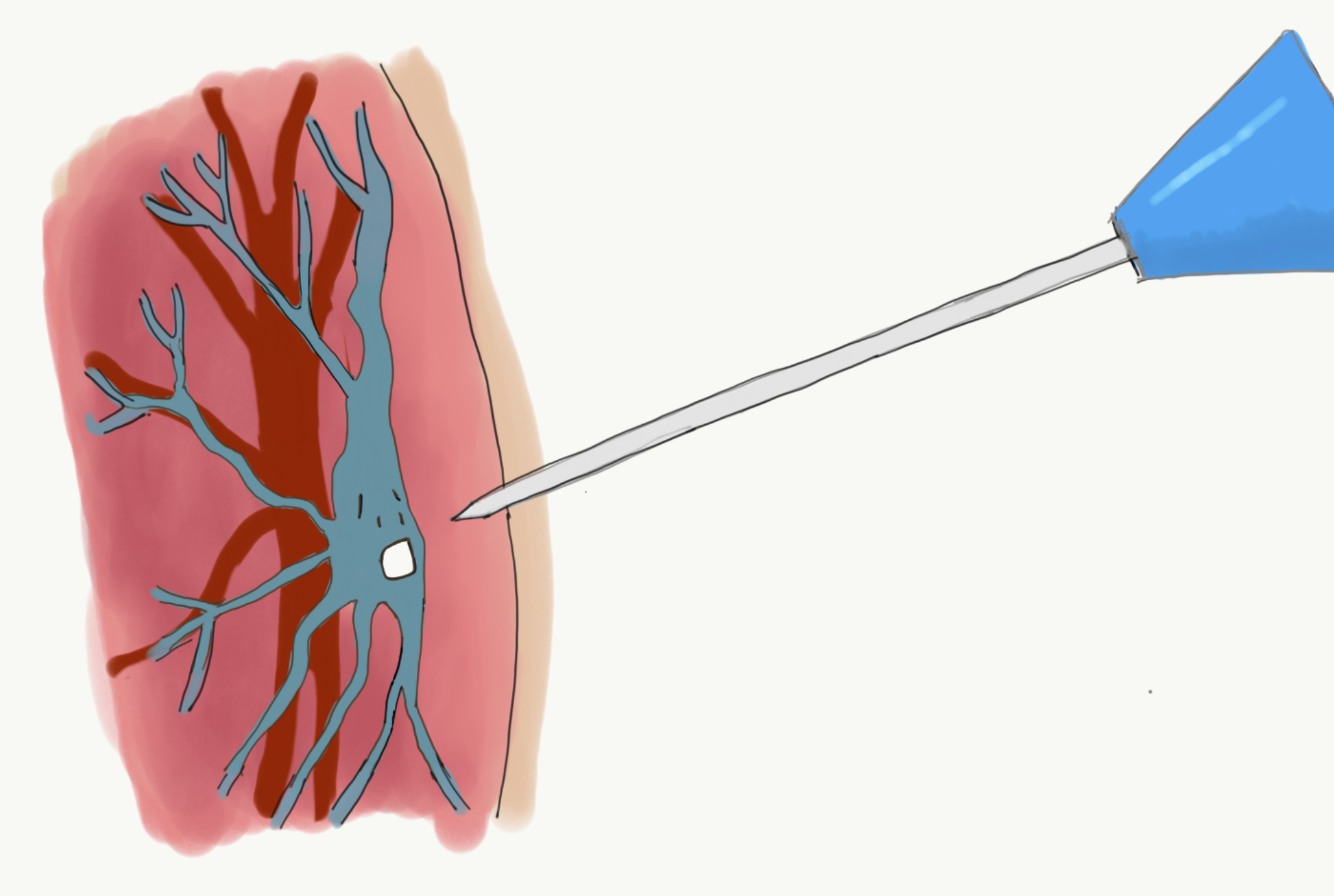
P.S. Check out the new illustration by Sapphire on my earlier April 2017 post called ‘My Veins Fear Needles!’. It’s fab!
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Nutrition for Cancer Tagged with: Cancer, Eating, Food, Myeloma, Nutrition, Organic, Sugar, Supplements, vegetable, weight
It happened again today. Someone said the wrong thing. They didn’t mean to. They just didn’t seem to think. In that moment, it seemed that it was important for them to say what they wanted to say, so they said it. Important to them, not me; about them, not me.
I’m sure they didn’t mean to have their words upset me. But they did. A nurse started telling me HER chemo story, uninvited. Maybe she thought I wanted to hear it, after all she went through ‘hers’ seven years ago and she’s still here; that’s something I’d want to hear, right? Wrong. I didn’t want to hear it. I very rarely want to hear others’ stories.
I didn’t want to hear it this morning when I was running later than usual and really looking forward to a much overdue call with one of my best friends, someone who always makes me feel great, even when we have talked through sad stuff or tough stuff or vented or cried together. I didn’t want to hear someone else’s story when I hadn’t asked to know. The nurse looked at me, waiting expectedly for me to ask more about it. I just wanted her to get on with taking my blood so I could get out there and make my call. She looked again. Today, I had no energy to ‘hold her off’ so I obliged. I smiled and she launched in with more detail and things I didn’t really hear, other than the ‘good luck’ at the end. Another thing I don’t always want to hear.
I couldn’t get out of there fast enough. On top of that the needle had hurt this morning; maybe because she was so focussed on offloading her story instead of taking my blood? She didn’t know how her words landed, she probably thought she was doing me a favour and on another day, maybe I would have wanted to hear her and chat away. How could she know?

Scared
I’m scared to write this blog. I think it might be taken the wrong way. Friends, family, blog readers might stop being in touch or think I’m ungrateful for all the contact, well wishes and kindness they have provided to me. Nothing could be farther from the truth. I am so grateful. I’m deeply astonished at the amazing volume, regularity and quality of support, I have received. Although, it hasn’t always been easy to receive it. I have often felt overwhelmed, sometimes smothered and obligated to respond.
There, I said it. Gosh it is hard to say in my head, let alone see it in black and white. I feel instantly guilty…and yet, honest. When I started this blog journey, I said I aimed to be real with it and share good, bad, up, down, times. I almost didn’t do that with these feelings as they feel so controversial, so risky, potentially hurtful; the last thing I want to be, ever.
I feel very vulnerable. What if you don’t understand? What if I describe how I have felt at certain times and I lose you; the very people, the very support, that has helped me get this far, that has helped me to feel loved and never alone. What do I do if after reading this, you don’t reach out again? Or don’t want to? Or think of me differently? Or want to reach out and are left not knowing if you should, or what to say?
I do hope you read to the end of this post. I do hope you understand.
Please believe me when I say I am not talking about any one person; I’m not. I’m trying to share the cumulative impact of these interactions and understand my own response to them. I’m trying to share the overall feelings, curious, conflicted, visceral and confusing reactions I have experienced, when people have been in touch, shown they care, tried to help and asked ‘How are you?’.
How are you?
Ahh, those three little words…’How are you?’. Now that I have cancer, the words, the question, feel so loaded, so complicated, with no easy answer. Being asked ‘How are you?’ isn’t helpful to me. Not right now anyway.
How on earth could you know that? It’s not your fault that you have asked me, many times, that very question; it’s a natural question to ask. You couldn’t know, that I am only now observing my reaction to the words, reflecting and working out for myself, that these three words are some of the most unhelpful to hear. Today, I was reminded that my experience and feelings about this, are not unique. Surveys show one of the things people living with cancer find unhelpful is people asking, ‘How are you?’.
Fair
One of the reasons I set up the blog, is so I didn’t have to say the same thing, give the same update, say the same answer to the question ‘How are you?’ to everyone who was kind enough to whatsapp, call, message, facebook, email. I hoped people might head to the blog, get a feel for how I was doing and leave a short comment if they wanted to. In that way, they would let me know what they thought of the blog or let me know they were thinking of me.
This wasn’t fair. It wasn’t fair on you. My hope, expectation, request doesn’t reflect human nature. Everyone has different ways they prefer to do things, different ways of communicating, connecting, showing love, showing kindness. It’s natural to do things your way. It is also fine for me to try and figure out, how, I can make that work for me too.
Please don’t…
Friends, family, strangers, clinicians, all say the ‘wrong’ thing, quite often. You don’t mean to. Most of the time I’m convinced people are well intentioned or at the very least trying to manage their discomfort in the best way they can in the moment. I also know, I have done the very same thing; been well intentioned but said something to someone or offered unsolicited advice that they may have found unhelpful, inappropriate or ignorant. When it has happened to me in the past, such as during an IVF journey, it used to make me angry. Now I’m living with Myeloma, when people say the wrong thing, anger is only one reaction amongst a range of reactions, and the whole communication situation – well, it’s weird.
Sometimes it is easy to let comments, questions and advice go. Other times, most times, communication is fraught. I want to scream; ‘not every cancer is the same’, ‘no one person’s treatment and side effects and best decisions for them are the same’, ‘No, I’m still doing chemo’, ‘ I don’t want to give you a low down on my treatment cycle in the middle of the street or maybe ever’, ‘Read my blog!’. Please don’t tell me about the person you know who has the same cancer as me and who is ‘still going after 20 years’ (I’ve been told by the people who know, clinicians and studies, that I have considerably fewer years left in my life so how is hearing that, going to help me? And my diagnosis came at stage two, was the person you are speaking about diagnosed at stage 1 or pre-stage 1, with smouldering Myeloma? How is that like me? Oh, you don’t know? Then how do you know it is even remotely relevant or interesting to me?
Please ‘don’t tell me you were speaking to a friend and their cousin has Myeloma and you can get me their number if I want’, In fact, please don’t even hint you’ve been talking about me with someone else (because that feels creepy) even though, I get this too, is a natural thing to do….and unless we are in the middle of a discussion and are talking about nutrition and supplements, or even then, please don’t suggest the next fad in ‘cancer cures’ (I’ve done my due diligence and made my choices).
Please don’t say, ‘it’s not your time’. As much as I’d like to believe it too, hearing it makes me feel very strange. On one hand, I want to agree and step into that idea, after all I have already said previously, I was sitting with the idea that my specific Cancer would become a chronic illness rather than terminal in my life time. On the other hand, I get washed with anger and want to say ‘wake up’, ‘get real’, ‘if you can’t accept it, how do you think I feel? How do you think I’ll ever accept it?’ Or ‘I’m accepting it, why can’t you?’
I just wonder what it would be like if a good friend instead said to me, ‘sh@t, x years, that’s a real nasty one, do you fancy talking through how you going to spend those years? What the years will involve treatment wise, how much time that will take up (that you know about now) and what you might want to do when you are not at hospital or having treatment? Do you want some help to work that out? and…’I know you might not know right now or have the energy to think about it but please when you can, say how I can help make the years the best they can be’. This would be helpful, I think. I won’t know until it happens. What I do know is that the conversations I have had, along these lines, with these questions, felt; useful, helpful, hopeful and realistic. Thank you.
I read this back and I fear I sound petty. Does it? The feelings are real, I can’t stop them. Like thoughts, they just show up. What do I do with them? For a short time, I felt less conflicted, less weird, when I realised my feelings are experienced by other people with cancer. Macmillan is working on a media project which will look at the social experiences of people affected by cancer and recently asked, ‘What they are tired of hearing about cancer?’ A flood of responses poured in and were so achingly honest. I was surprised at how many people felt like I did and how many also felt conflicted by their feelings. My heart poured out for them because I ‘got it’; then I remembered I was one of them. My heart pours out for me too….and then it retreats, curls up in a corner, getting ready for whatever comes next.
Grateful
I’m going to say it again, in case you have forgotten: I love that some of you are taking an interest in Myeloma and taking the time to find out more about it. I don’t expect everyone to do that. I am so grateful for the good intention when people say things or get me a number or offer advice. I am grateful for people wanting me to feel there is hope, that there are things out there that may help me feel better, wanting me to hear of others’ good fortune and hope that I experience the same. I am grateful. However, my gratitude seems to get overshadowed by other experiences; anger, irritation, desperation for quiet, peace, no demands, no messages that require an answer and these are followed by guilt, confusion, being scared. I don’t know what to ask of you, regarding communication. I know my need might change day to day and what is unhelpful in one moment, might be what I crave the next week. I’m scared to feel alone; I risk pushing you away by writing this post.

About me or about you?
Life has been so socially busy since my diagnosis, I have had to laugh. Why wasn’t I going out, meeting up, going away on breaks with friends as much before all of this happened? Why now? Is it because I want to ‘pack in time’ with the great people in my life? ‘Grab it while I can’ and in case, I become so ill that I can’t see my friends? Well yes, that’s part of it though only a small part as I’m not initiating many of the social arrangements at this stage. Do people need a fix of me? Surely not; I’m not that interesting! (I’m not fishing for a compliment here). Do they need to check and see for themselves that I really am OK right now? Do they simply want to show they are there for me? Or do they want to check in with Si, see that he is doing OK, for themselves, and because I asked them to, in the beginning, when all this crazy cancer-ness began.
Or…is the contact all about you? Is it you, the gorgeously caring soul who wants to do the right thing? Or be seen to do the right thing? Or to do, what you think you might like done, if roles were reversed, if you had cancer?. Being vulnerable again and at the risk of losing you, I am going to say that sometimes it feels demanding; “When can we next meet up?”; “Do you want to go away for the weekend?”; “Do you want to go abroad with us?”; “What can I make you?”; “Can I get you something?” Yes, I do want to go abroad, but I can’t fly right now; Yes, I do want to meet up though I have seen you twice in the last month and I need to see others too. I have smaller windows of non-hospital, non-chemo recovery time and less energy than I used to have right now. When I do have time and energy, I want to see all my good friends and family. If I see you, you my good friend, again, who do I not see, and when do I rest?
Or is it conflicting and demanding for me, because I never want to say ‘No’? In case next month, I’m not well enough to be social. I say ‘Yes’ and then get irritated that I can’t find time to rest. In an earlier post, I recommended being social while you can, as connection is good for the soul. I may need to revise this recommendation as not all socialising is helpful, inspiring or a good thing: sometimes choosing rest, quiet, alone time is important too. Also, I don’t want to miss out on experiences, so if you suggest a meet up (in the UK) to go and do something new or go somewhere new to do something fun, then I would love to say ‘Yes’. Rather than demanding, right now those suggestions seem to land differently; they feel nourishing, a chance to maximise quality of life.
What is helpful?
What is helpful communication wise? I’m not exactly sure yet. I think being in touch (please don’t stop being in touch!) but let me know how YOU are doing…rather than asking about me. I am having to focus so much on myself right now, my health, my hospital appointments, my food intake, water intake, my mental health, on an hour to hour basis, that it is so so so lovely to hear YOUR news, even a snippet, an up, a down, both or simply letting me know a ‘is what it is’ in your life, is great.
Selfishness
So…here’s another question / dilemma that has been whizzing around in my head, ‘ What level of selfishness is acceptable in a person living with cancer?’. Is it a different level for those living without cancer, major illness, other major challenge? How much selfishness is the right amount? How selfish am I allowed to be? What is my selfishness allowed to look like? Is it selfish, to want a fair amount of space, alone time, no sadness from others, people to be decisive and direct, to not have my time wasted (remember, its short and precious)?
Is it selfish to not answer messages that have questions in them, any question, and particularly ‘how are you?’ because it feels like a demand, something someone needs from me. Is this whole post selfish? Am I a selfish person? Have I always been selfish? Is selfish different from self-focussed? Is it ok for me to be self-focussed right now? What is that allowed to look like? What is acceptable? Should I care? Yes. I’d stop being me, if I stopped caring what impact I was having on others. Whizzing around……
Psychology: Ready
There are helpful psychology theories and practices that I can apply to help myself with this. I’m not ready to do that right now. Readiness is crucial in psychology. Seeking help is often a first sign of readiness, though even then, someone can still need time to become ready to explore difficult feelings or be willing to make changes in line with their goals. I haven’t sought help from myself yet. As I consider it now, briefly, two main ideas cross my mind; compassion for me – my feelings are normal and valid and, no-one can ‘make’ me feel a certain way. When I hear something unhelpful, I may react with a range of feeling and thoughts. I still have control; I can still choose what I focus on, choose my lasting reaction and choose how my day is impacted by what I hear. More about this in another post. I’m still ‘in the experience’ right now and not quite ready to seek help.
Please remember
I’m strong and I’m not.
I’m working out what is helpful and unhelpful. I don’t expect you to know. Its ok to ask.
I need space. I still need you.
I’m scared how you will feel when you read this post but I can’t control your feelings and how you choose to react; they’re your feelings, your choices.
I do hope you choose to stay in touch.
Resources that might help you to know what people with cancer find helpful and unhelpful
BBC: Things not to say to someone with cancer. A great little video. http://bbc.in/2kK4Wst
Acknowledgements:
Si, A, S and J who encourage me to be me every step of the way.
Image (sleeping me): B
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Psychology for Cancer Tagged with: Cancer, communication, grateful, helpful, Myeloma, Psychology, ready, say, scared, unhelpful

Causes, Choices, Control and Change.
Now that I have circumnavigated the first two months of treatment, with a focus on doing what had to be done, I notice the question of ‘Why Me?’ popping into my head more often. I think about causes, choices, control, and change. What caused my Myeloma? Why Myeloma and not another cancer? Did my past choices cause my Cancer? What can I control now? How do I keep control? What should I change about myself? What should I change about my lifestyle? If I make changes, will my prognosis be the same? Will changes really make a difference? Or will I just think changes make a difference? Will I create false hope? If I make a bunch of changes and my cancer gets worse, or remission is short or only the same as every other person with Myeloma, will I feel cheated, get depressed, wish I’d just carried on as normal and not changed anything? Are thinking about causes, control, changes and choices like a mouse going down a tunnel with no cheese? Which are illusions, which are realities?
Ultimately, the question I was asking myself was: “Should I change my terrain?”
The main areas of terrain I was considering were:
- Nutrition
- Chemicals/Toxins
- Mobile Phone / Technology
- Mindfulness and Meditation
Why the focus on these areas of terrain?
I was considering these areas as they made sense to me as possible areas for change. The science, while not based on randomised control trials, is compelling and pointed out in an easy-to-read book called Anti-Cancer, a new way of life by Dr David Servan-Schreiber (who also had cancer).
After all, it is unlikely that there will ever be large swathes of money on offer for randomised control trials (RCTs) about Nutrition for Cancer when Big Pharmaceutical companies are competing for the same pot of money for their new drug… or when the findings from Nutrition trials may potentially show there is no longer a need for an existing drug that makes someone a whole lot of profit right now.
Don’t get me wrong, I am very grateful for Big Pharma, their RCTs and their drugs; they are helping me to kick Myeloma into remission. I am however, a strong advocate for a holistic approach; an informed meld between medical and non-medical models, especially as the West learns to give more open consideration to healing and health strategies that have been used by non-Western cultures for centuries.
Particularly too, as while Cancer effects people of all ages and socio-economic status, it appears to predominantly be…drum roll… a first world country problem. Why is it that the rates of Cancer are very high in some countries (France, Denmark, USA, New Zealand and UK) in comparison to other countries (Japan, India, Oman). Why is it that more developed countries fair worse than less developed? 268 cases of cancer were diagnosed per 100,000 in more developed regions, compared to 148 in less developed regions in 2012, with an exception being the non-melanoma skin cancer rates which were higher for less developed countries. Why do other countries have crazily high rates of people with major illnesses other than cancer, such as heart disease (Turkey, Russia)?
Although diagnosis and recording systems availability and accuracy may influence data, could it be that certain types of stress, food, individualistic societies or combinations of these are also having an impact on cancer rates?
‘Why Me?’
I indulged my ‘Why Me?’ for a short time and asked: “Was it because I had chronic stress for years?” Was it because, before changing career, I had worked in contracts for telcos and banks, with constant tight deadlines, crazy commutes (5 hours a day at one stage) and a feeling of always having too much work and never getting it done? I wondered, did I get cancer because I’d lived on coffee for years, eaten too much chocolate, cake, biscuits, drunk too much alcohol during my twenties (and thirties)? Or was it because I was too analytical, too ‘in my head’, ‘too something’? Was this my path, my destiny? Was I meant to learn something? Be something from this experience? Did I even believe in paths, fate, non-fate?….and so like any normal human ‘bean’, I dwelt for a little while and still do occasionally. And, this IS a tunnel with no cheese. This conversation with myself, doesn’t serve me. I don’t hang out there for long.
A reality.
We (me, my medical team, the fatalists and non-fatalists in my life) don’t really know the answer to Why Me? When I asked the medical team, if anything I had done, used or consumed, caused the Myeloma, they insisted there is no evidence for links between my list and people getting Myeloma. I rattled off: stressful jobs; caffeine and alcohol; supplements; skin potions and lotions; whacky, at the time, spa treatments; and, multiple surgeries (involving though not exclusively, three knee and a number of IVF related invasions).
It may be something I’ve done or something I haven’t done, something about my biological make up, my vulnerabilities, the years of chronic stress, the coffee or lack of coffee (I went without for a year) or some very specific combination of some, or all of these, in very specific amounts of severity, for a specific duration. Are you noticing the complexity of ‘cause’ here? No one really knows and no one may ever know. There may be some amazing medical breakthrough in two years, 4 months and 6 days, when someone is studying finger surgery and discovers something new about Myeloma, that then leads to a randomised control trial or DNA discovery that may indicate some possible cause of Myeloma.
Let’s face it – right now, what we know is, Myeloma strikes at random and in general, men over 70 years old seem to get struck a little more than most. Until such time, as some crazy discovery is discovered, there isn’t much point me thinking about ‘Why Me’?
Yet…..
I can’t help thinking, if I don’t change something about: how I was living, what I was putting into my body and, how I was thinking, I’ll invite the status quo or a repeat performance. That is, won’t I be inviting Myeloma to return once it is in remission, if I don’t change the terrain in which it developed, ran amok and was diagnosed? This is the possible illusion as today’s reality (medical knowledge) indicates Myeloma always ultimately returns and people living with Myeloma eventually stop responding to treatment (drugs and transplants). However, making changes and choices, help a person to feel in control of their day to day or to feel they have some control over their illness: another illusion? Possibly…but….
What if changing my terrain works?
If I changed my terrain and it didn’t change my prognosis or my response to treatment, I would be disappointed but at least I’d know, I had done the best I could. No regrets. Or would I think, sh*t I should have just had chocolate fudge cake whenever I felt like it, three coffees a day (and thrown in margaritas and champagne regularly) because it probably didn’t make a blind bit of difference?!
Regret?
But what if it did work? What if I changed my terrain: changed my nutrition; removed my mobile phone from the bedroom; replaced my cleaning products with eco friendly, less toxic ones; used only ‘safe plastic’ or glass to store food; changed my skin care products to chemical free, natural ones; and practiced mindfulness and meditated regularly? What if, after all of these changes my response rate to Chemotherapy was excellent and my remission period was longer than average. Wouldn’t the choices, changes and exerted control be worth it?! SO, what choice do I have, really? How will I know what difference change makes, without making change? If I don’t make all the changes, all at once, don’t I risk missing out on gaining the full benefit, if there is a benefit to be gained?
Causes, Choices, Control and Change – both illusions and realities.
I don’t know the cause of Myeloma. I don’t know if my past choices had any influence over whether I got Myeloma or not. I don’t know if my present and future choices will influence how my Myeloma treatment, prognosis and experience will play out. The only thing I do know, is that I can choose to change and making changes may help me to feel in control. Taking control and making changes may have a positive impact on my lifetime outcome and my experience of the cancer journey or at the very least it may help me to feel some semblance of lack of regret.
Psychology – Choices.
What I also know (though it can be easy to forget this) is that I can always choose to review my choices regularly and change them. No one is stuck with a choice. It might feel like it yet we make dozens of choices every minute of the day – which direction in which to move, what to say, to eat or not eat if we have food, where to look. We can keep choosing even about the big-ticket items in our life. Just because we take one path doesn’t mean we can’t, pause, reflect, review and make another choice or reaffirm the choice we have made.
For example, each day for the last six weeks, I chose not to have coffee. Now, I’m going to get one, and savour it. You might say, well if you were a smoker trying to quit smoking, a choice of having one cigarette may be a poor choice. I might choose to agree. Alternatively, I might choose another tack and say that the smoker trying to give up who finds his/herself having one cigarette, could choose to not ‘beat their-self up over it’; they could choose to recommit to their goal of giving up and choose in each minute, to not have a cigarette. Better yet, they could also choose to make a positive healthy, non-cigarette involving choice, about what to do and where to place their attention. In other words, I would encourage positive choices that serve them and their goals.
Now relate this to Chemo and Changing My Terrain. Two months ago, I chose to start Chemo. Tomorrow, I might choose to stop. I could. I might. Right now, I have reviewed my choice and I am happy with my choice to do Chemo and be in a clinical trial. It doesn’t mean I can’t choose differently tomorrow, if I so wish. Let’s take a breather now; more about choices and attention later. Hmmmm, smell that coffee.

Acknowledgements:
World Cancer Research Fund International
http://www.wcrf.org/int/cancer-facts-figures/data-cancer-frequency-country
http://www.wcrf.org/int/cancer-facts-figures/comparing-more-less-developed-countries
World Health Organisation
http://www.who.int/nmh/countries/en/
Editorial help (any errors are solely my own): Simon Hayward and Belinda Marment
Illustration: Sapphire Weerakone
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Myeloma Treatment, Nutrition for Cancer, Psychology for Cancer Tagged with: Cancer, Cause, Change, Choice, Control, Lifestyle, Mobile, Myeloma, Nutrition, Terrain, Treatment, Why Me
It’s been hard to write the blog in week’s four, five and six of Chemo; I didn’t know where to start, there didn’t seem to be time, and I was worrying. Even Music didn’t show up much; I didn’t hear it or go looking for it – strange.

I started to worry about having little time; not time on this earth but time during the day to do all the things I needed to do. Sound familiar? I have learned over the years that when I worry about not having enough time, it usually means I am probably trying to do too much and am not getting enough rest or chill space. I noticed too that when reminders popped up in my calendar to get some ‘headspace’ or do a visualisation, I was swiping them away and thinking I’ll do that later yet later never came. This worried me.
I wondered whether my blood test results for week four would not be as good as the previous weeks and imply that going away to Canada had been a bad call after all. It turned out this worry, while natural, was unfounded; my results showed more test results falling within the normal range than in the previous weeks and suggested my immune system was hanging in there – a good result.
I worried about an interaction with a Nurse and found myself feeling ‘told off’, then wondering if I was being over sensitive, or not sensitive enough to others. I felt guilty for coping well with and doing well on Chemo. The nurse had asked how I was doing and I had said something along the lines of “really well thanks” and “chemo had been quick today”. I heard a response of “well that’s not the case for everyone”.
Then a stream of thoughts flooded my mind;
- Sh*t, had I spoken too loudly?
- A lot of people look very ill and drained on the Chemo ward today, have I not thought of them? Should I think of them?
- I have answered honestly and positively; that’s what I committed to do throughout this process wherever possible.
Feeling a bit indignant, more thoughts rushed in;
- No, it’s fine for me to be positive after all it’s not my fault I’m doing well,
- Being positive is meant to help with healing so I’m not going to stop answering ‘I’m Doing Well’, when I am doing well.
Overnight and with reflection I decided I probably was being a bit sensitive and it was also fine to be positive. The following day I checked in with the nurse, who quickly reassured me that he had not thought I’d been insensitive to others on the ward at all. We cleared any misunderstanding and he reiterated how great it was that I was doing well. This frank discussion helped bring clarity and perspective to my thoughts. It stopped this worry completely. I’m glad I raised it with the nurse even though I was uncertain (and nervous) about what I might hear.

Despite this resolution, a residual sense of stress, worry and an over active adrenal system remained; the opposite of the many calm moments that I had been experiencing last month. The overall worrying continued.
My weight had dropped again to 66kg and I was struggling to eat enough calories. I often didn’t feel hungry but still tried to eat. I hoped my weight would stabilise and even climb back up to 68kg. That weight had felt comfortable while now I noticed I didn’t seem to have much padding, wondered if I really did have much of a reserve if I got an infection and I noticed I had lost muscle mass. The backs of my hands look like some very elderly person’s hands; dry and wrinkly despite the constant fluid intake. I worried that my weight would keep falling and my skin would get worse.
I worried about whether I should stick to the plan of not working for six months to focus on getting to remission as successfully as possible or to work while I still could. I worried about if I worked, would it be too stressful, leave me enough time to rest or feel like it’s getting in the way. I worried about not being able to work out how much work was too much, and for private practice whether enough work matched with breaking even financially. I worried about how to contain my clients’ concerns if my appearance changed with more chemo and how I provide a consistency of safe space for them if my medical appointments needed to change in the future. I worried and yet I missed making a difference and being the psychologist I know I can be.
To cap off the week, I finally had a long-awaited Ear, Nose and Throat appointment (yet another hospital visit) to check my possible hearing loss. This is something else I have been worried about for a long time and that has no doubt been bugging Si for years as I constantly ask him to repeat himself or need the TV volume well above the level he would choose. I had noticed my hearing was worse when; I’d find it difficult in crowded places (and with background noise) to hear the person I was standing next to and speaking with, or to hear what someone was saying if I couldn’t see their face and mouth. I noticed I had started guessing (not always accurately) what someone was saying.
For a psychologist; listening skills are imperative and before listening skills can be invoked one has to be able to hear! While I had rarely experienced these problems in one to one therapy sessions, I was concerned symptoms would get worse or impact my functioning. Sure enough I wasn’t dreaming this either; tests showed my hearing has deteriorated though is still in the mild loss range; inner ear cochlear deterioration so unrecoverable. This is essentially the kind of loss most people start experiencing from around 60 years old on…except I’m not 50 yet! I suspect I’m paying the price for good times; a burst ear drum while scuba diving as a teenager and damage from standing far too close to speakers at Fabric nightclub a few years back (ok, so quite a few years ago now).
So I’ve been worrying and it’s completely natural to worry. It is not helpful to dwell in worry or worry about things I can’t control so how do I let go of it? Worry is something I have helped many clients with over the last ten years so it is definitely time for some self-help. Below are the psychology tips and strategies I reminded myself to use.
Psychology – Overcoming and managing worry

What is Worry? How worry works.
Worry is a form of mental problem solving about potentially negative future events. It can be triggered by a variety of external events or from thoughts that just pop into your head. Worry is characterised by a lot of ‘what if’ questions. For example, ‘What if my Chemo doesn’t work?’ ‘What if my new boss doesn’t like me or think I’m good enough?’
Normal worry is usually short lived and leads to positive problem solving activities. Worry becomes unhelpful when it is about several things, is frequent and difficult to control or dismiss. We can think prolonged or frequent worry helps with problem solving, planning and preparation however worry breeds more worry (and anxiety) which prevents positive thinking and action.
Worrying can rob people of time. It’s exhausting and often leaves people feeling tense, with disturbed sleep, difficulties concentrating, and feeling irritable. While sometimes it can feel appropriate or necessary, worrying is exactly the opposite; it’s restrictive, and takes up time, attention and energy that could be spent on useful, enjoyable and meaningful activities.
Why do some people seem to worry more than others?
Worrying is human! The causes of are not clearly understood though it may be that a number of vulnerabilities increase the chance of developing a tendency to worry excessively; prolonged stress, past experiences of uncontrollable or traumatic events, an inherited biological disposition to experience negative emotions, learned messages from others that the world is unsafe or that worry is useful, and a coping style that involves avoiding challenges or situations where there is a chance of experiencing negative emotions (which prevents positive experience of coping and positive emotions).
Managing worry.
UNDERSTAND YOUR WORRY CYCLES – Understand your vicious cycles of anxiety and how avoidance contributes to anxiety. See the handout below (CCI – Vicious Cycle of Anxiety).
NOTICE YOUR PAYOFFS AND COSTS. Part of understanding your worry can be to notice if you are getting a pay-off from worrying, ‘buying into it’ and most importantly what the cost of the pay-off might be. Are you avoiding going out? You might get a pay-off of avoiding any negative emotions such as uncertainty of what will happen or be said when you see someone but you also miss out on the potential positive experiences; fun, laughter, connectedness or ease which going out may also provide. Also notice, where do you worry and what are you doing when you worry. For example, are you sitting down and telling yourself ‘you are worrying but getting rest at the same time’. Consider that your type of ‘sitting down’ in this instance is not truly restful and what it actually costs you is feeling rested. If you shifted your attention away from worry to giving yourself permission for genuine rest, and allowed yourself to do something enjoyable without the worrying in that same time, you are much more likely to feel rested and relaxed (and be better able to cope with normal levels of worry that we all experience).
Other practical strategies:
USE A WORRY TREE to identify where to put your attention so that you shift your attention to worries you can do something about and form a plan for rather than worries you have no control over. There is a link to a handout below
CHANGE “WHAT IF’ STATEMENTS TO ‘HOW’ STATEMENTS’. For example, instead of “what if Chemo doesn’t work?’ I might ask myself ‘How will I act if Chemo doesn’t work? How will I find out what action can be taken next?’
POSTPONE WORRY. This is where you give yourself permission to worry about a specific topic, at a particularly time later in the day, for a maximum duration of say 20 minutes). This way you are acknowledging your concern and allowing yourself to think about it for a contained amount of time without it taking over and impacting the rest of your day. Sometimes you may find the thing you were worrying about has resolved itself by the time the allotted worrying time has come around, or it looks completely different and isn’t as big of an issue as it seemed earlier or doesn’t have to be dealt with today after all.
Summary
These are just some tips for managing worry and there are others if these don’t work for you. Remember, while worry is normal, excessive worry can be gripping and creep up on anyone. Even when worry can feel like a good thing to do, it creates more anxiety. When it stops you from enjoying life or doing the things you want to do, worry is not your friend. Excessive worry can be overcome. Please try the strategies outlined above and the links to helpful handouts below. If you find them hard to do alone, do talk with your GP or ask a psychologist to help with gaining treatment or to work through the strategies with you.
Acknowledgements, Permissions and Helpful Handouts:
Centre for Clinical Interventions (CCI), Department of Health, Australia http://www.cci.health.wa.gov.au/
CCI Generalised Anxiety and Worry
http://www.cci.health.wa.gov.au/resources/infopax_doc.cfm?Mini_ID=46
CCI Vicious Cycle of Anxiety
http://www.cci.health.wa.gov.au/resources/docs/Info-Vicious%20Cycle%20of%20Anxiety.pdf
CCI Postponing Worry
http://www.cci.health.wa.gov.au/docs/ACF3D66.pdf
Get Self Help Get.gg – Worry Tree
https://www.getselfhelp.co.uk/docs/worrytree.pdf
Images: Simon Hayward
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Chemotherapy for Myeloma, Psychology for Cancer Tagged with: Cancer, Chemotherapy, Myeloma, Psychology, Worry
April 24th, 2017 by Janine
Aside from the Chemo, my body has consumed at least 534 medications and 825 supplements in the last 50 days….1359 pills in all.
I visited a well know artist with a gallery in South London. I tried to have an open mind but still came away not liking the art!
I did discover the gallery has an interesting cafe based on a pharmacy (and one of the artist’s famous pieces) with an array of pills show cased all over the walls. If I post pics of all of my pills do you think he’ll come after me for plagiarism?!
My average day….

I’m officially a pill popper!
Posted in Myeloma Treatment, Nutrition for Cancer Tagged with: Cancer, Medication, Myeloma, Pills, Supplements, Treatment, Vitamins
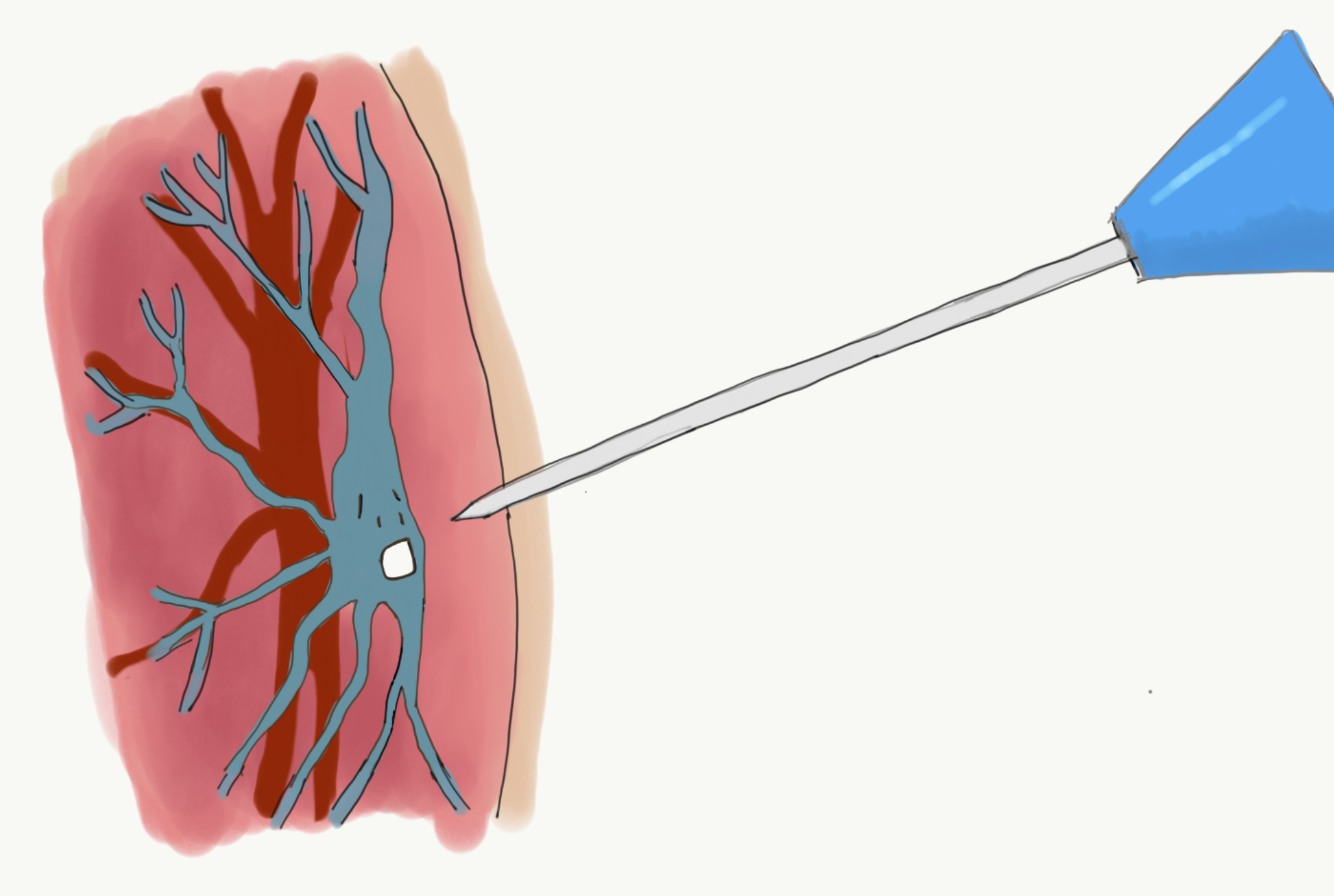
April 19th, 2017 by Janine
My veins are not playing ball. According to one Nurse they are spidery, superficial and collapse as soon as a needle comes near them. This is the accumulation effect of the Carfilzomib drug and not unexpected. I had hoped this side-effect may take a bit longer to kick in but hey I want the drug to work so I will take some of the after effects! For each needle insertion attempt that fails – is it Bad Karma? Maybe for my veering off course with my plans… the odd coffee, sip of alcohol, not enough rest…a fabulous slice of chocolate fudge cake on hubby’s birthday (hey I’m only human!).
On the first day of my veins playing ‘hide and seek’ (Nurse L’s description) and after two Nurses had taken two to three pin cushion moments on my arms (with my permission) they called in K. As he and Simon bantered about K being the ‘big gun’ and having a ‘big probe’, I discovered what K had brought with him was an ultrasound machine, and that he is one of the few (possibly only) Nurse trained on the Chemo day unit) in using ultrasound for finding veins. In that moment, I loved K; he found a vein quickly and had the cannula in my arm in a flash. The hours of trying to find a vein were not in vain!!
So yesterday when Nurse L said, ‘I’ve come to make friends with your veins’ I said ‘absolutely’ thinking that just because it been hard to find them last week didn’t mean it had to be hard again this week. Unfortunately, that was not the case and the ever-cautious Nurse L was wonderful and genuinely sorry it wasn’t going smoothly. My next request was, could we not muck around any further today please, and get K and his ultrasound. This is when I found out K wasn’t in. K of course is allowed a day off (or two!) however I was unimpressed that only one person can use the machine I need. I imagined that given they know of the accumulation effect of Chemo, I am not the first person to have elusive veins.
Nurse G said he was rusty on using the ultrasound but he’d give it a go. He showed me the images of my veins disappearing as soon as a gentle pressure from the probe was applied in my arm. He abandoned it and said he wasn’t confident enough to use it successfully. Good news though; he checked the back of my left arm and said he could see a vein. He checked whether it be ok to try otherwise they would probably have to insert a PICC line. I didn’t want a PICC line before absolutely necessary so I gave the go ahead, hoping like hell it would work. I could have kissed him, straight in, a little sore but the needle didn’t escape the vein; Si and I escaped the Chemo unit by 5pm.
Kicking in to rationale mode, I started thinking;
- It’s not my fault I need an ultrasound, or that only one Nurse seems to be able to do it; I will always need that Nurse to be available on my Chemo days
- The scenario above is not the Chemo Unit Nurses fault
- It is an unacceptable scenario
- I shouldn’t have to have a PICC line earlier than necessary just because it’s convenient for staff
Moving into problem solving mode; I decided I need to
Ask my consultant;
- How to resolve this; is there another nurse from another team who can be scheduled/ available?
- Can K be scheduled for my Chemo days (cover when he’s on leave)
- How quickly can another Nurse be trained to use ultrasound?
Also ask my consultant about below…
- How much does a private Nurse with right skills cost, can they attend NHS site, can they bring ultrasound machine or use NHS equipment (liability, insurance, clinical trial, other
PICC lines are peripherally inserted central catheters (long, flexible tubes) that are put into a large vein above the bend in the elbow, threaded into a vein until the tip sits in a large vein just above the heart. PICC lines can make things easier for Nurses and for me; it means there is always a line into a vein (with a removable cap) that enables a bag of intravenous drugs to be easily attached; there would no longer be a need to poke around with needles to put a cannula in or to take blood.

On the flip side, PICC lines stay in, require a local anaesthetic and chest X-ray (to check positioning) which are no big deal but are more procedures, and insertion may need to be done multiple times to get the right position. PICC lines get in the way of clothing, need cleaning and re-dressing weekly (Mondays would become even busier visits to hospital), the lines stay in for weeks or months, non-Chemo weeks would then involve visits to hospital. Finally, they are another daily reminder that I have cancer and how my life is different now. I knew i would happily have one when it’s necessary; it just doesn’t feel necessary yet when ultrasound searching for veins has worked.
Today was also a case in point for deferring PICC for as long as possible. I kept my arm and hand warm all morning, under two thermals and a glove. Nurse L found a vein first time. Lovely.
I was in and out of hospital in under two hours.
A tough week ended in A GOOD DAY!
Acknowledgements:
Co-Content: Hubby.
Image: Macmillan information sheet on PICC Lines
Illustration (Scaredy Vein): Sapphire Weerakone
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Chemotherapy for Myeloma Tagged with: Cancer, Cannula, Myeloma, Needles, PICC Line, Ultrasound
April 9th, 2017 by Janine
A cracking question
A cracking question and one that had crossed my mind when I first started learning about Myeloma. Most of us have heard of Leukemia, or know someone who has requested donations for a fun run they are doing in the name of a charity, supporting people living with Leukemia or sponsoring Leukemia research. It seems Myeloma and Lymphoma are less visible or talked about. To rectify this, please find a wee overview of their similarities and differences below.
Do keep your questions coming.
They are helpful to me and I am sure they may be helpful to others too. It is fine to ask; What is X?, How are you coping with Y? or Are you afraid of Z? All questions make me think, reflect and ensure I am staying informed and open with myself, and others, about all aspects of this journey. So seriously, even though you have heard it a million times before: No question is a silly question!
Differences and Similarities
Multiple myeloma and myeloid leukemia have much in common. The names are similar, because they are both cancers that start in the bone marrow. Many of the symptoms are similar, and even some of the same drugs are used to treat both diseases. However, they are two distinctly different entities. Multiple myeloma and myeloid leukemia involve different cell types; B plasma cells and myeloid line of cells respectively.
Lymphoma specifically affects the lymph nodes. The type of lymphoma is based on the origins of the cancer cells. Some start in the lymphatic system (Hodgkin’s), while others begin in the white blood cells (non-Hodgkin lymphomas).
Differences
| Topic |
Leukemia |
Multiple Myeloma |
Lymphoma |
| Stats (UK, 2014):
New Cases
Deaths
Survival (10+yrs, 2011)
Preventable Cases |
9534
4584
46%
15%
|
5501
2928
33%
<1% |
2106 (H) 13605 (n-H)
355 (H) 4801 (n-H)
80% (H) 63% (n-H)
45% (H) 6% (n-H) |
| Cell type |
Myeloid |
Type B Plasma |
|
| Arises in |
Bone Marrow and Blood in form of Myeloblasts and Lymphoblasts |
Myelium
(Bone marrow) |
Lymphatic system, or white blood cells |
| Some Symptoms |
|
Bone Fractures |
|
|
Risk Factors associated with an increased chance of developing the disease
|
· Pre-existing blood disorders eg. MDS or MPN
· Age – most forms of leukaemia are more common in older people. The main exception to this is ALL in which peak incidence is in children
|
· Age—Most myeloma patients are between 50 and 70 years old
· Race— Almost twice as common in Black populations as it is in White and Asian populations
|
For Hodgkin’s;
· Infection with infectious mononucleosis
· Age—Hodgkin’s disease occurs most often in people between ages 15 and 34, and in people over the age of 55
· Epstein-Barr virus may increase a person’s risk of Hodgkin’s disease
· Acquired immune deficiency syndrome (AIDS)
For Non-Hodgkin’s;
· Unprotected exposure to strong sunlight
· A high-fat, low-fibre diet
· Smoking or the use of tobacco products
· Excessive alcohol consumption
· Organ transplantation
· Infections with human immunodeficiency virus (HIV) or human T-cell leukemia/lymphoma virus (HTLV-1)
· Infections with malaria
· A history of infectious mononucleosis (caused by an infection with the Epstein-Barr virus)
· Helicobacter pylori (H. pylori) bacterium, which has been identified as a cause of stomach ulcers
|
Similarities
| Topic |
Leukemia |
Multiple Myeloma |
Lymphoma |
| Blood cancer |
X |
X |
X |
| Scientists unsure why one person is more likely than another to get this cancer |
X |
X |
X |
| Exact causes unknown |
X |
X |
X |
| Starts in bone marrow |
X |
X |
|
| Some Symptoms (e.g. anaemia, bruising and infections) |
X |
X |
|
| Drug treatment (some) |
X |
X |
|
| Risk factors associated with an increased chance of developing the disease |
· Exposure to high levels of radiation and particular chemicals, especially benzene and some chemotherapy drugs
· Particular genetic disorders e.g. Down’s syndrome
· Gender— more common in men than in women
|
· Exposure to certain workplace chemicals and large amounts of radiation
· Gender— more common in men than in women
· A family history of myeloma
|
For Non-Hodgkin’s;
· Environmental factors such as radiation, chemicals, and infections
· Genetic disease of the immune system
· Gender—more common in men than in women
· Family history of lymphoma, particularly brothers and sisters
|
Leukemia (also spelled Leukaemia)
Leukemia is cancer of the blood cells, usually affecting the white blood cells, which causes these cells to not work properly.
There are four main types of leukemia; acute myelogenous leukemia (AML), chronic myelogenous leukemia (CML), acute lymphocytic leukemia (ALL), or chronic lymphocytic leukemia (CLL). In addition to these, there are other types and subtypes of leukemia.
Leukemia can occur in either the lymphoid or myeloid white blood cells. Cancer that develops in the lymphoid cells is called lymphocytic leukemia. Cancer that develops in the myeloid cells is called myelogenous leukemia. The disease can be either acute (begins abruptly and is usually short lived) or chronic (persists for a long period of time).
Acute leukemia involves new or immature cells, called blasts, which remain very immature and cannot perform their functions. The blasts increase in number rapidly, and the disease progresses quickly. In chronic leukemia, there are some blasts present, but they are more mature and can perform some of their functions. The cells grow more slowly so the disease progresses gradually.
Myeloma
Multiple myeloma is a type of cancer that affects certain white blood cells called plasma cells. Plasma cells are part of the immune system, which helps protect the body from infection and disease. Like all white blood cells, plasma cells begin their development in the bone marrow, the soft, spongy tissue that fills the centre of most bones.
When cancer involves plasma cells, the body keeps producing more and more of these cells. The unneeded plasma cells—all abnormal and exactly alike—are called myeloma cells. Myeloma cells tend to collect in the bone marrow and in the hard, outer part of the bones. Patients with multiple myeloma suffer bone fractures in parts of the bone where the cancer is lodged. Ninety percent of patients have cancer lodged in different bony locations, which is why it is referred to as “multiple.”
In most cases, people who develop multiple myeloma have no clear risk factors. Scientists believe the disease may be the result of several factors (known and/or unknown) acting together. (Wish I knew what they were so I avoid the same combination of factors again!!!)
The name “myeloma” is somewhat deceiving because this cancer does not involve myeloid cells. It gets its name because it arises in the myelium, or bone marrow.
Lymphoma
Lymphoma is a type of cancer that originates in the lymphatic system. There are two main types of lymphoma. Hodgkin’s lymphoma (or Hodgkin’s disease) and non-Hodgkin’s lymphomas.
Hodgkin’s lymphoma or Hodgkin’s disease causes the cells in the lymphatic system to abnormally reproduce, eventually making the body less able to fight infection. All other types of lymphoma are called non-Hodgkin’s lymphomas.
Cancers that spread to lymph nodes from other parts of the body are not lymphomas.
The lymphatic system, the tissues and organs that produce, store, and carry white blood cells that fight infections and other diseases, includes the bone marrow, spleen, thymus, lymph nodes, and lymphatic vessels. It is important for filtering germs and cancer cells from various parts of the body. Lymphoid tissue is found in many places throughout the body, including lymph nodes, the thymus (found behind the chest bone and in front of the heart), the spleen (on the left side of the abdomen next to the stomach), the tonsils and adenoids, in the bone marrow, and scattered within other systems such as the digestive and respiratory systems.
Acknowledgements:
Cancer Research UK
http://www.cancerresearchuk.org/health-professional/cancer-statistics
Sylvester Comprehensive Cancer Centre (University of Miami Health System) http://sylvester.org/cancer/leukemia-lymphoma-and-myeloma/education/definition
Leukaemia Care
http://www.leukaemiacare.org.uk/
Multiple Myeloma Research Foundation MMRF
https://www.themmrf.org/
Livestrong
http://www.livestrong.com/article/215375-what-are-the-differences-between-multiple-myeloma-myeloid-leukemia/
Illustration: Sapphire Weerakone
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Diagnosis, Your Questions Tagged with: Cancer, Differences, Leukemia, Lymphoma, Myeloma, Similarities, Statistics